Ibuprofen
Advil | Advil Children's | Advil Children's Fever | Advil Infants' | Advil Junior Strength | Advil Migraine | ALIVIO | Caldolor | Children's Ibuprofen | ElixSure IB | Genpril | Ibren | IBU | Ibupak | Midol | Midol Cramps and Body Aches | Motrin | Motrin Children's | Motrin IB | Motrin Infants' | Motrin Junior Strength | Motrin Migraine Pain | PediaCare Children's Pain Reliever/Fever Reducer IB | PediaCare Infants' Pain Reliever/Fever Reducer IB | Samson-8 | Toxicology Saliva Collection | Last revised on November 27, 2025
Read moreIndications/Dosage
altitude sickness prophylaxis
arthralgia
common cold
cystic fibrosis
dental pain
dysmenorrhea
fever
frostbite
gout
gouty arthritis
headache
juvenile rheumatoid arthritis (JRA)/juvenile idiopathic arthritis (JIA)
migraine
mild pain
moderate pain
musculoskeletal pain
osteoarthritis
pericarditis
rheumatic arthritis
rheumatoid arthritis
severe pain
For the treatment of rheumatoid arthritis (RA) and juvenile rheumatoid arthritis (JRA)/juvenile idiopathic arthritis (JIA)*
Oral dosage (tablets or suspension)
Adults:
300 mg PO 4 times daily or 400 to 800 mg PO 3 to 4 times daily. Max: 3,200 mg/day.[30569] [44120] [44121]
Children and Adolescents:
30 to 50 mg/kg/day PO in 3 to 4 divided doses (Max: 800 mg/dose).[44121] [54023] [55102] [55106] [55107] Lower dose to smallest effective dose once clinical effect is attained. Patients with milder disease may be adequately treated with 20 mg/kg/day.[44121] [54023]
For the treatment of osteoarthritis*
Oral dosage (tablets or suspension)
Adults:
300 mg PO 4 times daily or 400 to 800 mg PO 3 to 4 times daily. Max: 3,200 mg/day.[30569] [44120] [44121]
For the treatment of dysmenorrhea*
Oral dosage (tablets or suspension)
Adults:
800 mg PO once, then 400 to 800 mg PO every 8 hours as needed.[71619] [71620] The FDA-approved dosage is 400 mg PO every 4 to 6 hours as needed. Max: 3,200 mg/day.[30569]
Adolescents:
800 mg PO once, then 400 to 800 mg PO every 8 hours as needed.[71619] [71620]
Oral dosage (OTC tablets)
Adults:
200 to 400 mg PO every 4 to 6 hours as needed. Max: 1,200 mg/day. Discontinue use if pain gets worse or lasts more than 10 days.[55095]
Children and Adolescents 12 to 17 years:
200 to 400 mg PO every 4 to 6 hours as needed. Max: 1,200 mg/day. Discontinue use if pain gets worse or lasts more than 10 days.[55095]
For the treatment of moderate to severe pain as an adjunct to opioids*
Intravenous dosage
Adults:
400 to 800 mg IV every 6 hours as needed. Max: 3,200 mg/day.[35893]
Children and Adolescents 12 to 17 years:
400 mg IV every 4 to 6 hours as needed. Max: 2,400 mg/day.[35893]
Infants and Children 6 months to 11 years:
10 mg/kg/dose (Max: 400 mg/dose) IV every 4 to 6 hours as needed. Max: 40 mg/kg/day or 2,400 mg/day, whichever is less.[35893]
Infants 3 to 5 months:
10 mg/kg/dose (Max: 100 mg/dose) IV as a single dose.[35893]
For the treatment of mild pain to moderate pain, including minor aches and pains associated with arthralgia, dental pain, headache, musculoskeletal pain (including backache), and/or the common cold*
NOTE: Use weight to determine pediatric dosage when possible.[55086]
for the treatment of mild to moderate pain*
Oral dosage (tablets)
Adults:
400 mg PO every 4 to 6 hours as needed. Max: 3,200 mg/day. In controlled analgesic clinical trials, doses more than 400 mg were no more effective than the 400 mg dose.[30569]
Oral dosage (suspension)
Infants and Children 6 months to 2 years:
10 mg/kg/dose PO every 6 to 8 hours. Max: 40 mg/kg/day.[44121]
Intravenous dosage
Adults:
400 to 800 mg IV every 6 hours as needed. Max: 3,200 mg/day.[35893]
Children and Adolescents 12 to 17 years:
400 mg IV every 4 to 6 hours as needed. Max: 2,400 mg/day.[35893]
Infants and Children 6 months to 11 years:
10 mg/kg/dose (Max: 400 mg/dose) IV every 4 to 6 hours as needed. Max: 40 mg/kg/day or 2,400 mg/day, whichever is less.[35893]
Infants 3 to 5 months:
10 mg/kg/dose (Max: 100 mg/dose) IV as a single dose.[35893]
for the treatment of minor aches and pains associated with arthralgia, dental pain, headache, musculoskeletal pain (including backache), and/or the common cold*
Oral dosage (OTC tablets)
Adults:
200 to 400 mg PO every 4 to 6 hours as needed. Max: 1,200 mg/day.[55095]
Children and Adolescents 12 to 17 years:
200 to 400 mg PO every 4 to 6 hours as needed. Max: 1,200 mg/day.[55095]
Oral dosage (OTC tablets or suspension)
Children 11 years or weighing 72 to 95 pounds:
300 mg PO every 6 to 8 hours as needed. Max: 1,200 mg/day.[66830] [66831]
Children 9 to 10 years or weighing 60 to 71 pounds:
250 mg PO every 6 to 8 hours as needed. Max: 1,000 mg/day.[66830] [66831]
Children 6 to 8 years or weighing 48 to 59 pounds:
200 mg PO every 6 to 8 hours as needed. Max: 800 mg/day.[66830] [66831]
Children 4 to 5 years or weighing 36 to 47 pounds:
150 mg PO every 6 to 8 hours as needed. Max: 600 mg/day.[66830] [66831]
Children 2 to 3 years or weighing 24 to 35 pounds:
100 mg PO every 6 to 8 hours as needed. Max: 400 mg/day.[66830] [66831]
Oral dosage (OTC concentrated drops)
Children 12 to 23 months or weighing 18 to 23 pounds:
75 mg PO every 6 to 8 hours as needed. Max: 300 mg/day.[66832]
Infants 6 to 11 months or weighing 12 to 17 pounds:
50 mg PO every 6 to 8 hours as needed. Max: 200 mg/day.[66832]
For the treatment of fever*
NOTE: Use weight to determine pediatric dosage when possible.[55086]
Oral dosage (OTC tablets)
Adults:
200 to 400 mg PO every 4 to 6 hours as needed. Max: 1,200 mg/day. Discontinue use if fever gets worse or lasts more than 3 days.[55095]
Children and Adolescents 12 to 17 years:
200 to 400 mg PO every 4 to 6 hours as needed. Max: 1,200 mg/day. Discontinue use if fever gets worse or lasts more than 3 days.[55095]
Oral dosage (OTC tablets or suspension)
Children 11 years or weighing 72 to 95 pounds:
300 mg PO every 6 to 8 hours as needed. Max: 1,200 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66830] [66831]
Children 9 to 10 years or weighing 60 to 71 pounds:
250 mg PO every 6 to 8 hours as needed. Max: 1,000 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66830] [66831]
Children 6 to 8 years or weighing 48 to 59 pounds:
200 mg PO every 6 to 8 hours as needed. Max: 800 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66830] [66831]
Children 4 to 5 years or weighing 36 to 47 pounds:
150 mg PO every 6 to 8 hours as needed. Max: 600 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66830] [66831]
Children 2 to 3 years or weighing 24 to 35 pounds:
100 mg PO every 6 to 8 hours as needed. Max: 400 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66830] [66831]
Oral dosage (OTC concentrated drops)
Children 12 to 23 months or weighing 18 to 23 pounds:
75 mg PO every 6 to 8 hours as needed. Max: 300 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66832]
Infants 6 to 11 months or weighing 12 to 17 pounds:
50 mg PO every 6 to 8 hours as needed. Max: 200 mg/day. Discontinue use if no relief within 24 hours or if fever gets worse or lasts more than 3 days.[66832]
Oral dosage (suspension)
Infants and Children 6 months to 2 years:
5 to 10 mg/kg/dose PO every 6 to 8 hours. Max: 40 mg/kg/day.[44121]
Intravenous dosage
Adults:
400 mg IV once, then 400 mg IV every 4 to 6 hours or 100 to 200 mg IV every 4 hours as needed. Max: 3,200 mg/day.[35893]
Children and Adolescents 12 to 17 years:
400 mg IV every 4 to 6 hours as needed. Max: 2,400 mg/day.[35893]
Infants and Children 6 months to 11 years:
10 mg/kg/dose (Max: 400 mg/dose) IV every 4 to 6 hours as needed. Max: 40 mg/kg/day or 2,400 mg/day, whichever is less.[35893]
Infants 3 to 5 months:
10 mg/kg/dose (Max: 100 mg/dose) IV as a single dose.[35893]
For the treatment of cystic fibrosis† to slow the rate of decline in pulmonary function*
Oral dosage
Adults:
20 to 30 mg/kg/dose (Max: 1,600 mg/dose) PO twice daily, initially. Adjust dose to maintain a peak serum concentration of 50 to 100 mcg/mL.[24179] [54023] [55084] [56767]
Children and Adolescents 6 to 17 years:
20 to 30 mg/kg/dose (Max: 1,600 mg/dose) PO twice daily, initially. Adjust dose to maintain a peak serum concentration of 50 to 100 mcg/mL.[24179] [54023] [55084] [56767] Guidelines recommend the chronic use of oral ibuprofen for children 6 to 17 years with cystic fibrosis who have an FEV1 of more than 60% predicted.[56767] [68127]
For the treatment of frostbite†*
Oral dosage
Adults:
6 mg/kg/dose PO twice daily, initially. May increase the dose as needed. Max: 600 mg PO 4 times daily. Continue until frostbite wound is healed or surgical management occurs (typically for 4 to 6 weeks). Guidelines suggest ibuprofen to inhibit harmful prostaglandins, which can cause vasoconstriction, dermal ischemia, and further tissues damage.[71081]
For the acute treatment of migraine*
Oral dosage
Adults:
200 to 400 mg PO as a single dose.[64565] [66574] Guidelines classify ibuprofen as having established efficacy for the treatment of acute migraine.[64565] [69288]
Children† and Adolescents†:
7.5 to 10 mg/kg/dose (Max: 600 mg/dose) PO as a single dose.[21333] [24245] [64587] Guidelines recommend ibuprofen as an initial treatment option to reduce pain in children and adolescents with migraine.[64587]
For the treatment of acute or recurrent pericarditis†*
for the treatment of acute pericarditis†*
Oral dosage
Adults:
600 to 800 mg PO every 8 hours for 1 to 2 weeks, then decrease dose by 200 to 400 mg/day every 1 to 2 weeks in combination with colchicine.[67418] [71453]
Children and Adolescents:
30 to 50 mg/kg/day PO divided every 8 hours for 1 to 4 weeks. Max: 2.4 g/day. Consider tapering dose gradually every 1 to 2 weeks.[67418] [67419]
for the treatment of recurrent pericarditis†*
Oral dosage
Adults:
600 to 800 mg PO every 8 hours for at least 2 to 4 weeks, then decrease dose by 200 to 400 mg/day every 1 to 2 weeks in combination with colchicine. Dose range: 1,200 to 2,400 mg/day.[60439] [67418] [71453]
Children and Adolescents:
30 to 50 mg/kg/day PO divided every 8 hours for at least 2 to 4 weeks in combination with colchicine. Max: 2.4 g/day. Consider tapering dose gradually every 1 to 2 weeks.[67418] [67419]
For the treatment of acute gout† or acute gouty arthritis†*
Oral dosage
Adults:
800 mg PO 3 to 4 times daily as needed until the attack has subsided.[64373]
For the treatment of rheumatic arthritis†*
Oral dosage
Adults:
200 to 400 mg PO 3 times daily, initially. May increase the dose up to 2,400 mg/day based on clinical response and tolerability. Treat for 1 month or until inflammation has subsided.[72005] [72025]
Infants, Children, and Adolescents:
5 to 10 mg/kg/dose (Max: 400 mg/dose) PO 3 times daily, initially. May increase the dose up to 2,400 mg/day based on clinical response and tolerability. Treat for 1 month or until inflammation has subsided.[72005] [72025]
For altitude sickness prophylaxis†*
Oral dosage
Adults:
600 mg PO every 8 hours starting the day before ascent and continuing for 2 to 3 days after reaching the target altitude or until descent is initiated.[72681] [72682]
Maximum Dosage Limits:*
•Adults
3,200 mg/day PO/IV for Rx-only products; 1,200 mg/day PO for non-prescription use.
•Geriatric
3,200 mg/day PO/IV for Rx-only products; 1,200 mg/day PO for non-prescription use.
•Adolescents
17 years: 3,200 mg/day PO/IV for Rx-only products; 1,200 mg/day PO for non-prescription use.
13 to 16 years: 50 mg/kg/day PO (Max: 3,200 mg/day) and 2,400 mg/day IV for Rx-only products; 1,200 mg/day PO for non-prescription use.
•Children
12 years: 50 mg/kg/day PO (Max: 3,200 mg/day) and 2,400 mg/day IV for Rx-only products; 40 mg/kg/day PO (Max: 1,200 mg/day) for non-prescription use.
1 to 11 years: 50 mg/kg/day PO (Max: 3,200 mg/day) and 40 mg/kg/day IV (Max: 2,400 mg/day) for Rx-only products; 40 mg/kg/day PO (Max: 1,200 mg/day) for non-prescription use.
•Infants
6 to 11 months: 40 mg/kg/day PO and 40 mg/kg/day IV (Max: 2,400 mg/day) for Rx-only products; 40 mg/kg/day PO (Max: 300 mg/day) for non-prescription use.
3 to 5 months: 10 mg/kg/day IV (Max: 100 mg/day). Safety and efficacy of other dosage forms have not been established.
1 to 2 months: Safety and efficacy have not been established.
•Neonates
Safety and efficacy have not been established.
Patients with Hepatic Impairment Dosing*
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Patients with Renal Impairment Dosing*
Avoid use of ibuprofen in patients with advanced renal disease unless the benefits are expected to outweigh the risks of worsening renal function.[35893] If use is necessary, monitor renal function closely.[44120] Guidelines recommend the following:
GFR 30 to 59 mL/minute/1.73 m2: Avoid use in patients with intercurrent disease that increases the risk of acute kidney injury. Prolonged therapy is not recommended. GFR less than 30 mL/minute/1.73 m2: Avoid use.[62206]
Intermittent hemodialysis
No dosage adjustment is necessary.[32569]
No dosage adjustment is necessary.[32569]
No dosage adjustment is necessary.[32569]
How Supplied
Ibuprofen Chewable tablet
Advil Children's 50mg Chewable Tablet (00573-0177) (GlaxoSmithKline Consumer Healthcare) (2008-02-28T00:00:00)
Ibuprofen Chewable tablet
Motrin Children's 50mg Chewable Tablet (Grape) (50580-0907) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division) (2006-09-30T00:00:00)
Ibuprofen Chewable tablet
Motrin Children's 50mg Chewable Tablet (Orange) (50580-0205) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division) (2009-02-02T00:00:00)
Ibuprofen Chewable tablet
Advil Junior Strength 100mg Chewable Tablet (00573-0179) (GlaxoSmithKline Consumer Healthcare) (2010-12-10T00:00:00)
Ibuprofen Chewable tablet
Advil Junior Strength 100mg Chewable Tablet (Grape) (00573-0179) (Haleon US Holdings LLC)
Ibuprofen Chewable tablet
CVS Children's Ibuprofen 100mg Chewable Tablet (Orange) (69842-0706) (CVS Health)
Ibuprofen Chewable tablet
CVS Children's Ibuprofen 100mg Chewable Tablet (Orange) (69842-0329) (CVS Health)
Ibuprofen Chewable tablet
CVS Children's Ibuprofen 100mg Chewable Tablet (Orange) (70677-0072) (McKesson Corporation) (2024-02-10T00:00:00)
Ibuprofen Chewable tablet
CVS Junior Ibuprofen 100mg Chewable Tablet (Grape) (59779-0521) (CVS Health) (2017-09-30T00:00:00)
Ibuprofen Chewable tablet
CVS Junior Ibuprofen 100mg Chewable Tablet (Grape) (59779-0521) (CVS Health)

Ibuprofen Chewable tablet
CVS Junior Ibuprofen 100mg Chewable Tablet (Orange) (59779-0461) (CVS Health) (2023-05-01T00:00:00)
Ibuprofen Chewable tablet
Equaline Children's Ibuprofen 100mg Chewable Tablet (Grape) (41163-0521) (Albertson's, Inc)
Ibuprofen Chewable tablet
Equate Children's Ibuprofen 100mg Chewable Tablet (Grape) (49035-0521) (Wal-Mart Stores, Inc.)
Ibuprofen Chewable tablet
GNP Children's Ibuprofen 100mg Chewable Tablet (Grape) (46122-0632) (AmerisourceBergen Corporation)
Ibuprofen Chewable tablet
GNP Children's Ibuprofen 100mg Chewable Tablet (Orange) (46122-0617) (AmerisourceBergen Corporation)
Ibuprofen Chewable tablet
GNP Junior Ibuprofen 100mg Chewable Tablet (Grape) (46122-0010) (AmerisourceBergen Corporation)
Ibuprofen Chewable tablet
GNP Junior Ibuprofen 100mg Chewable Tablet (Orange) (24385-0546) (AmerisourceBergen Corporation)
Ibuprofen Chewable tablet
GoodSense Children's Ibuprofen 100mg Chewable Tablet (Orange) (00113-2461) (Perrigo Company)
Ibuprofen Chewable tablet
GoodSense Junior Ibuprofen 100mg Chewable Tablet (00113-0461) (Goodsense a Division of Perrigo)
Ibuprofen Chewable tablet
Health Mart Junior Ibuprofen IB 100mg Chewable Tablet (62011-0334) (McKesson Corporation) (2019-03-23T00:00:00)
Ibuprofen Chewable tablet
Health Mart Junior Strength Ibuprofen IB 100mg Chewable Tablet (Orange) (62011-0367) (McKesson Corporation) (2020-05-06T00:00:00)
Ibuprofen Chewable tablet
Ibuprofen 100mg Chewable Tablet (71205-0423) (Proficient Rx LP)
Ibuprofen Chewable tablet
Junior Ibuprofen 100mg Chewable Tablet (00904-5691) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2009-11-10T00:00:00)
Ibuprofen Chewable tablet
Kroger Junior Strength Ibuprofen 100mg Chewable Tablet (Orange) (30142-0461) (The Kroger Co.)
Ibuprofen Chewable tablet
Leader Children's Ibuprofen 100mg Chewable Tablet (Grape) (70000-0239) (Cardinal Health, Inc.)
Ibuprofen Chewable tablet
Leader Junior Ibuprofen 100mg Chewable Tablet (Grape) (37205-0852) (Cardinal Health, Inc.)
Ibuprofen Chewable tablet
Leader Junior Ibuprofen 100mg Chewable Tablet (Orange) (37205-0402) (Cardinal Health, Inc.) (2017-12-04T00:00:00)
Ibuprofen Chewable tablet
Leader Junior Ibuprofen 100mg Chewable Tablet (Orange) (70000-0240) (Cardinal Health, Inc.) (2022-07-11T00:00:00)
Ibuprofen Chewable tablet
Motrin Children's 100mg Chewable Tablet (Grape) (00045-0909) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2022-07-04T00:00:00)
Ibuprofen Chewable tablet
Motrin Children's 100mg Dye-Free Chewable Tablet (Grape) (00045-0932) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2022-07-04T00:00:00)
Ibuprofen Chewable tablet
Motrin Junior 100mg Chewable Tablet (Grape) (00045-0909) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2012-06-01T00:00:00)
Ibuprofen Chewable tablet
Motrin Junior 100mg Chewable Tablet (Orange) (00045-0494) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2012-06-01T00:00:00)
Ibuprofen Chewable tablet
Publix Junior Ibuprofen 100mg Chewable Tablet (56062-0461) (Publix Super Markets, Inc)
Ibuprofen Chewable tablet
RITE AID Junior Ibuprofen 100mg Chewable Tablet (null) (Rite Aid Corp)

Ibuprofen Chewable tablet
RITE AID Junior Ibuprofen 100mg Chewable Tablet (Grape) (null) (Rite Aid Corp)

Ibuprofen Chewable tablet
Sunmark Junior Ibuprofen IB 100mg Chewable Tablet (49348-0639) (McKesson Corporation) (2020-03-28T00:00:00)
Ibuprofen Chewable tablet
Top Care Junior Ibuprofen 100mg Chewable Tablet (36800-0461) (Topco Associates LLC)
Ibuprofen Chewable tablet
Walgreens Children's Ibuprofen 100mg Chewable Tablet (Grape) (11917-0107) (Walgreens Co.)
Ibuprofen Chewable tablet
Walgreens Junior Ibuprofen 100mg Chewable Tablet (Orange) (null) (Walgreens Co.)
Ibuprofen Oral capsule
Motrin IB 200mg Gelcap (50580-0770) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division) (2010-04-21T00:00:00)
Ibuprofen Oral capsule
Wal-Profen 200mg Capsule (00363-0038) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Liqui-Gel (00573-0169) (GlaxoSmithKline Consumer Healthcare) (2016-10-16T00:00:00)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Liqui-Gel (00573-0169) (GlaxoSmithKline Consumer Healthcare)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Liqui-Gel (00573-0149) (Haleon US Holdings LLC)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Liqui-Gel (00573-0169) (Haleon US Holdings LLC)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Liqui-Gel Packet (00573-0149) (GlaxoSmithKline Consumer Healthcare) (2008-04-29T00:00:00)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Migraine Capsule (00573-0168) (Haleon US Holdings LLC)
Ibuprofen Oral capsule, liquid filled
Advil 200mg Minis Liqui-Gel (00573-1769) (Haleon US Holdings LLC)
Ibuprofen Oral capsule, liquid filled
Advil Migraine 200mg Liquid Filled Capsule (00573-0168) (Haleon US Holdings LLC)

Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0197) (CVS Health) (2018-08-31T00:00:00)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59726-0120) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59726-0121) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (null) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0197) (CVS Health) (2018-08-31T00:00:00)

Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0197) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0108) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0197) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0197) (CVS Health)
Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (69842-0745) (CVS Health)

Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (69842-0745) (CVS Health)

Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Liquid Filled Softgel (59779-0197) (CVS Health)

Ibuprofen Oral capsule, liquid filled
CVS Ibuprofen 200mg Softgel (59726-0122) (CVS Health)

Ibuprofen Oral capsule, liquid filled
Equate Ibuprofen 200mg Mini Softgel (49035-0381) (Wal-Mart Stores, Inc.)
Ibuprofen Oral capsule, liquid filled
Foster & Thrive Ibuprofen 200mg Liquid-Filled Softgel (70677-1114) (McKesson Corporation) (2023-06-21T00:00:00)

Ibuprofen Oral capsule, liquid filled
Foster & Thrive Ibuprofen 200mg Liquid-Gel Capsule (70677-1282) (McKesson Corporation)

Ibuprofen Oral capsule, liquid filled
Foster & Thrive MINIS Ibuprofen 200mg Liquid Filled Softgel (70677-1113) (McKesson Corporation) (2023-10-18T00:00:00)

Ibuprofen Oral capsule, liquid filled
GNP Ibuprofen 200mg Mini Softgel (46122-0593) (AmerisourceBergen Corporation)
Ibuprofen Oral capsule, liquid filled
GNP Ibuprofen 200mg Softgel (24385-0499) (AmerisourceBergen Corporation)
Ibuprofen Oral capsule, liquid filled
GNP Ibuprofen 200mg Softgel (46122-0530) (AmerisourceBergen Corporation)
Ibuprofen Oral capsule, liquid filled
GNP Ibuprofen 200mg Softgel (46122-0530) (AmerisourceBergen Corporation)
Ibuprofen Oral capsule, liquid filled
GNP Ibuprofen 200mg Softgel (46122-0580) (AmerisourceBergen Corporation)
Ibuprofen Oral capsule, liquid filled
GoodSense Ibuprofen 200mg Liquid Filled Softgel (50804-0199) (Geiss, Destin & Dunn, Inc.)
Ibuprofen Oral capsule, liquid filled
GoodSense Ibuprofen 200mg Liquid Filled Softgel (00113-0298) (Goodsense a Division of Perrigo)
Ibuprofen Oral capsule, liquid filled
Health Mart Ibuprofen 200mg Softgel (62011-0016) (McKesson Corporation) (2018-11-07T00:00:00)
Ibuprofen Oral capsule, liquid filled
Ibuprofen 200mg Liquid Caps (00904-5903) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2010-02-28T00:00:00)
Ibuprofen Oral capsule, liquid filled
Ibuprofen 200mg Liquid Caps (00536-3603) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2018-06-06T00:00:00)
Ibuprofen Oral capsule, liquid filled
Ibuprofen 200mg Liquid Caps (00536-1147) (Rugby Laboratories a Division of The Harvard Drug Group, LLC)
Ibuprofen Oral capsule, liquid filled
Ibuprofen 200mg Liquid Capsule (69230-0146) (Camber Consumer Care, Inc.)
Ibuprofen Oral capsule, liquid filled
Ibuprofen 200mg Liquid Capsule (72865-0132) (XL Care Pharmaceuticals, Inc)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (70000-0571) (Cardinal Health Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (70000-0571) (Cardinal Health Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (37205-0328) (Cardinal Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (37205-0736) (Cardinal Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (37205-0736) (Cardinal Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (70000-0360) (Cardinal Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (70000-0360) (Cardinal Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (70000-0360) (Cardinal Health, Inc.) (2022-09-09T00:00:00)
Ibuprofen Oral capsule, liquid filled
Leader Ibuprofen 200mg Softgel (70000-0571) (Cardinal Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Midol 200mg Liquid Gel Capsule (12843-0536) (Bayer Corp Consumer Care Div)
Ibuprofen Oral capsule, liquid filled
Motrin Ibuprofen 200mg Softgel (00045-0409) (Janssen Pharmaceuticals, Inc.)
Ibuprofen Oral capsule, liquid filled
Premier Value Ibuprofen 200mg Softgel (null) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral capsule, liquid filled
Premier Value Ibuprofen 200mg Softgel (68016-0626) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral capsule, liquid filled
Quality Choice Ibuprofen 200mg Liquid Filled Softgel (63868-0427) (Chain Drug Marketing Association)

Ibuprofen Oral capsule, liquid filled
Quality Choice Ibuprofen 200mg Liquid Filled Softgel (63868-0428) (Chain Drug Marketing Association)
Ibuprofen Oral capsule, liquid filled
Quality Choice Ibuprofen 200mg Softgel (63868-0470) (Chain Drug Marketing Association)
Ibuprofen Oral capsule, liquid filled
Quality Choice Ibuprofen 200mg Softgel (35515-0952) (Chain Drug Marketing Association)
Ibuprofen Oral capsule, liquid filled
Quality Choice Ibuprofen 200mg Softgel (83324-0206) (Chain Drug Marketing Association)

Ibuprofen Oral capsule, liquid filled
Quality Choice Ibuprofen Dye-Free 200mg Liquid Filled Softgel (63868-0805) (Chain Drug Marketing Association)
Ibuprofen Oral capsule, liquid filled
RITE AID Ibuprofen 200mg Softgel (null) (Rite Aid Corp)

Ibuprofen Oral capsule, liquid filled
RITE AID Ibuprofen 200mg Softgel (null) (Rite Aid Corp)

Ibuprofen Oral capsule, liquid filled
RITE AID Ibuprofen 200mg Softgel (11822-0789) (Rite Aid Corp)
Ibuprofen Oral capsule, liquid filled
RITE AID Ibuprofen 200mg Softgel (11822-0100) (Rite Aid Corp)
Ibuprofen Oral capsule, liquid filled
RITE AID Ibuprofen 200mg Softgel (11822-0733) (Rite Aid Corp)
Ibuprofen Oral capsule, liquid filled
RITE AID Ibuprofen 200mg Softgel (11822-0302) (Rite Aid Corp)
Ibuprofen Oral capsule, liquid filled
Sunmark Ibuprofen 200mg Softgel (70677-0046) (McKesson Corporation) (2023-11-29T00:00:00)
Ibuprofen Oral capsule, liquid filled
Today's Health Ibuprofen 200mg Softgel (null) (Today's Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Today's Health Ibuprofen 200mg Softgel (null) (Today's Health, Inc.)
Ibuprofen Oral capsule, liquid filled
Wal-Profen 200mg Softgel (null) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Wal-Profen 200mg Softgel (null) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Wal-Profen 200mg Softgel (11917-0050) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Capsule (11917-0102) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0121) (Walgreens Co)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0749) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0945) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0945) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0945) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0945) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-1610) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-1610) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-1610) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-1610) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-1610) (Walgreens Co.)

Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0221) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0221) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0221) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0221) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0221) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Ibuprofen 200mg Softgel (00363-0222) (Walgreens Co.)
Ibuprofen Oral capsule, liquid filled
Walgreens Migraine Relief 200mg Softgel (00363-0240) (Walgreens Co.)

Ibuprofen Oral drops, suspension
Advil Infants' Concentrated 50mg/1.25ml Drops (Grape) (00573-0173) (GlaxoSmithKline Consumer Healthcare) (2020-06-30T00:00:00)
Ibuprofen Oral drops, suspension
Advil Infants' Concentrated 50mg/1.25ml Drops (White Grape) (00573-0191) (GlaxoSmithKline Consumer Healthcare) (2009-06-28T00:00:00)
Ibuprofen Oral drops, suspension
Advil Infants' Concentrated 50mg/1.25mL Drops (White Grape) (00573-0191) (GlaxoSmithKline Consumer Healthcare)
Ibuprofen Oral drops, suspension
Advil Infants' Concentrated 50mg/1.25mL Drops (White Grape) (00573-0191) (Haleon US Holdings LLC)
Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25ml Concentrated Drops (Berry) (59779-0057) (CVS Health)

Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (59779-0255) (CVS Health) (2018-10-31T00:00:00)
Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (null) (CVS Health)
Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (59779-1252) (CVS Health) (2013-03-01T00:00:00)
Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (59779-1252) (CVS Health)
Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (59779-0995) (CVS Health)
Ibuprofen Oral drops, suspension
CVS Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (59779-0313) (CVS Health)
Ibuprofen Oral drops, suspension
Equaline Infants' Ibuprofen 50mg/1.25mL Drops (Berry) (41163-0057) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral drops, suspension
Equaline Infants' Ibuprofen 50mg/1.25mL Drops (Berry) (41163-0255) (Albertson's, Inc)
Ibuprofen Oral drops, suspension
Equate Infants' Ibuprofen 50mg/1.25ml Suspension (Berry) (49035-0125) (Wal-Mart Stores, Inc.) (2020-05-30T00:00:00)
Ibuprofen Oral drops, suspension
Foster & Thrive Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (70677-1144) (McKesson Corporation)
Ibuprofen Oral drops, suspension
GNP Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (24385-0550) (AmerisourceBergen Corporation) (2024-02-18T00:00:00)
Ibuprofen Oral drops, suspension
GNP Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (24385-0550) (AmerisourceBergen Corporation)
Ibuprofen Oral drops, suspension
GoodSense Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (00113-0057) (Goodsense a Division of Perrigo)
Ibuprofen Oral drops, suspension
Health Mart Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (62011-0012) (McKesson Corporation) (2022-06-24T00:00:00)
Ibuprofen Oral drops, suspension
Health Mart Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (62011-0004) (McKesson Corporation) (2022-06-24T00:00:00)
Ibuprofen Oral drops, suspension
Ibuprofen 50mg/1.25ml Drops (00904-5463) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral drops, suspension
Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (63868-0076) (Chain Drug Marketing Association)
Ibuprofen Oral drops, suspension
Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (45802-0057) (Perrigo Pharmaceuticals Company) (2025-07-01T00:00:00)
Ibuprofen Oral drops, suspension
Infants' Ibuprofen 50mg/1.25ml Concentrated Suspension Drops (Berry) (71205-0110) (Proficient Rx LP)
Ibuprofen Oral drops, suspension
Infants' Ibuprofen 50mg/1.25ml Concentrated Suspension Drops (Berry) (45963-0125) (Teva/Actavis US)
Ibuprofen Oral drops, suspension
Leader Infants' Ibuprofen 50mg/1.25ml Concentrated Drops (Berry) (37205-0646) (Cardinal Health, Inc.) (2018-03-27T00:00:00)
Ibuprofen Oral drops, suspension
Leader Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (37205-0436) (Cardinal Health, Inc.)
Ibuprofen Oral drops, suspension
Leader Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (70000-0298) (Cardinal Health, Inc.)
Ibuprofen Oral drops, suspension
Leader Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (70000-0307) (Cardinal Health, Inc.) (2021-03-13T00:00:00)
Ibuprofen Oral drops, suspension
Motrin Infants' 50mg/1.25ml Suspension Drops (Berry) (00045-0198) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2012-10-10T00:00:00)
Ibuprofen Oral drops, suspension
Motrin Infants' 50mg/1.25ml Suspension Drops (Berry) (00045-0524) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2012-05-14T00:00:00)
Ibuprofen Oral drops, suspension
Motrin Infants' 50mg/1.25mL Suspension Drops (Berry) (50580-0100) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division)
Ibuprofen Oral drops, suspension
Motrin Infants' 50mg/1.25mL Suspension Drops (Berry) (50580-0100) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral drops, suspension
Motrin Infants' 50mg/1.25mL Suspension Drops (Berry) (50580-0198) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral drops, suspension
PediaCare Infants' Pain Reliever/Fever Reducer IB 50mg/1.25ml Concentrated Drops (Berry) (null) (Medtech Products, Inc., a subsidiary of Prestige Consumer Healthcare) (2013-01-01T00:00:00)
Ibuprofen Oral drops, suspension
Premier Value Infants' Ibuprofen 50mg/1.25ml Concentrated Drops (Berry) (68016-0025) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral drops, suspension
Publix Infants' Profen IB 50mg/1.25ml Drops (Berry) (56062-0057) (Publix Super Markets, Inc)
Ibuprofen Oral drops, suspension
Quality Choice Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (35515-0965) (Chain Drug Marketing Association)
Ibuprofen Oral drops, suspension
RITE AID Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (null) (Rite Aid Corp)

Ibuprofen Oral drops, suspension
RITE AID Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (null) (Rite Aid Corp)
Ibuprofen Oral drops, suspension
Sunmark Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (49348-0374) (McKesson Corporation) (2024-10-30T00:00:00)
Ibuprofen Oral drops, suspension
Sunmark Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (49348-0642) (McKesson Corporation) (2024-09-20T00:00:00)
Ibuprofen Oral drops, suspension
Top Care Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (36800-0057) (Topco Associates LLC)
Ibuprofen Oral drops, suspension
Top Care Infants' Ibuprofen 50mg/1.25mL Concentrated Suspension (Berry) (36800-0255) (Topco Associates LLC)
Ibuprofen Oral drops, suspension
Walgreens Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (00363-0057) (Walgreens Co.)

Ibuprofen Oral drops, suspension
Walgreens Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (00363-0255) (Walgreens Co.)

Ibuprofen Oral drops, suspension
Walgreens Infants' Ibuprofen 50mg/1.25mL Concentrated Drops (Berry) (00363-8139) (Walgreens Co.)
Ibuprofen Oral drops, suspension
Walgreens Infants' Ibuprofen 50mg/1.25mL Drops (00363-0057) (Walgreens Co.)
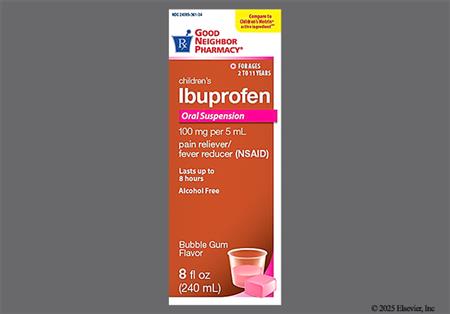
Ibuprofen Oral suspension
Advil Children's 100mg/5ml Suspension (Fruit) (00573-0170) (Haleon US Holdings LLC)
Ibuprofen Oral suspension
Advil Children's 100mg/5ml Suspension (Grape) (00573-0171) (Haleon US Holdings LLC)
Ibuprofen Oral suspension
Advil Children's 100mg/5ml Suspension (Raspberry) (00573-0174) (GlaxoSmithKline Consumer Healthcare) (2020-06-30T00:00:00)
Ibuprofen Oral suspension
Advil Children's Fever 100mg/5mL Suspension (Bubble Gum) (00573-0207) (Haleon US Holdings LLC)
Ibuprofen Oral suspension
Advil Children's Fever 100mg/5mL Suspension (Grape) (00573-0171) (GlaxoSmithKline Consumer Healthcare) (2020-06-30T00:00:00)
Ibuprofen Oral suspension
Advil Children's Fever 100mg/5mL Suspension (White Grape) (00573-0290) (Haleon US Holdings LLC)
Ibuprofen Oral suspension
Advil Children's Fever Sugar-Free 100mg/5mL Suspension (Berry) (00573-0232) (Haleon US Holdings LLC)
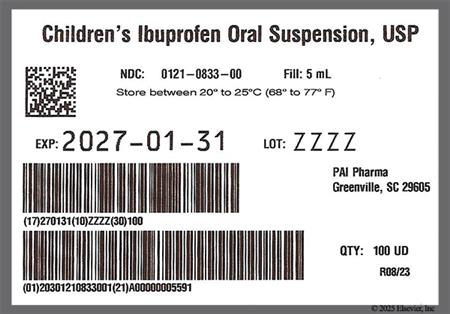
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (00121-0833) (Pharmaceutical Associates Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5ml Suspension (Berry) (00536-1081) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2017-04-27T00:00:00)
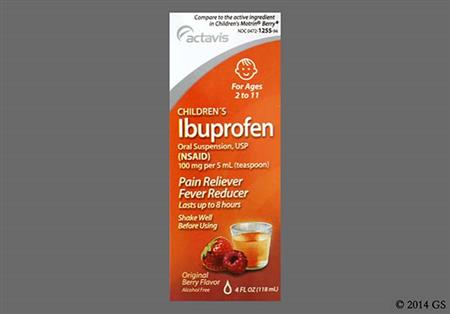
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5ml Suspension (Berry) (00472-1255) (Teva/Actavis US) (2006-06-21T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5ml Suspension (Berry) (00472-1255) (Teva/Actavis US) (2018-02-20T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (50090-3408) (A-S Medication Solutions LLC)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (50090-4129) (A-S Medication Solutions LLC)
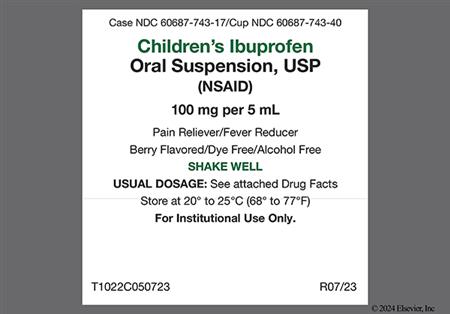
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (60687-0743) (American Health Packaging)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (68001-0435) (BluePoint Laboratories) (2023-05-30T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (68001-0521) (BluePoint Laboratories)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (63629-8540) (Bryant Ranch Prepack, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (69230-0308) (Camber Consumer Care, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (69230-0311) (Camber Consumer Care, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (61269-0761) (H2-Pharma, LLC) (2021-09-30T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00904-5309) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
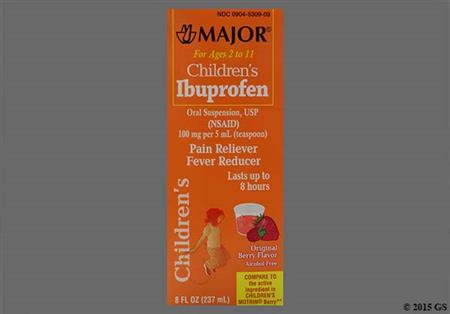
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00904-5309) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (45802-0897) (Padagis US LLC)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (45802-0897) (Perrigo Pharmaceuticals Company)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00121-1836) (Pharmaceutical Associates Inc.)

Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00121-0917) (Pharmaceutical Associates Inc.) (2023-01-05T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00121-1022) (Pharmaceutical Associates Inc.) (2025-10-13T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (68094-0494) (Precision Dose, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (68094-0600) (Precision Dose, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (68094-0037) (Precision Dose, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (68094-0494) (Precision Dose, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (69618-0078) (Reliable 1 Laboratories LLC )

Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (51672-5321) (Sun Pharmaceutical Industries, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (51672-2130) (Taro Pharmaceuticals USA Inc)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00472-1261) (Teva/Actavis US) (2018-04-11T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00472-1760) (Teva/Actavis US)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Berry) (00472-1761) (Teva/Actavis US)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Blue Raspberry) (00472-1764) (Teva/Actavis US)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Bubble Gum) (61269-0763) (H2-Pharma, LLC) (2021-12-22T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (69230-0310) (Camber Consumer Care, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (45802-0140) (Perrigo Pharmaceuticals Company)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (00472-1263) (Teva/Actavis US) (2018-02-05T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (00472-1763) (Teva/Actavis US)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5ml Suspension (Fruit) (00904-5464) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2011-02-14T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Grape) (69230-0309) (Camber Consumer Care, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Grape) (00904-5577) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Grape) (45802-0133) (Perrigo Pharmaceuticals Company)
Ibuprofen Oral suspension
Children's Ibuprofen 100mg/5mL Suspension (Grape) (00121-0914) (Pharmaceutical Associates Inc.)

Ibuprofen Oral suspension
Children's Ibuprofen 200mg/10mL Suspension (00121-1666) (Pharmaceutical Associates Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 200mg/10ml Suspension (Berry) (68094-0503) (Precision Dose, Inc.)
Ibuprofen Oral suspension
Children's Ibuprofen 200mg/10mL Suspension (Berry) (00121-2044) (Pharmaceutical Associates Inc.) (2025-10-13T00:00:00)
Ibuprofen Oral suspension
Children's Ibuprofen 200mg/10mL Suspension (Grape) (00121-1828) (Pharmaceutical Associates Inc.)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Berry) (59779-0897) (CVS Health) (2018-05-31T00:00:00)

Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Berry) (59779-0685) (CVS Health) (2019-09-30T00:00:00)

Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Berry) (59779-0897) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Berry) (59779-0897) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Berry) (59779-0685) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Berry) (59779-0685) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (59779-0166) (CVS Health) (2021-03-31T00:00:00)

Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (59779-0882) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (59779-0166) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Grape) (59779-0660) (CVS Health) (2017-05-31T00:00:00)

Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Grape) (null) (CVS Health)
Ibuprofen Oral suspension
CVS Children's Ibuprofen 100mg/5mL Suspension (Grape) (59779-0660) (CVS Health)

Ibuprofen Oral suspension
ElixSure IB 100mg/5ml Suspension (51672-2505) (TaroPharma ) (2005-03-03T00:00:00)
Ibuprofen Oral suspension
ElixSure IB 100mg/5mL Suspension (null) (Moberg Pharma NA formerly Alterna LLC)
Ibuprofen Oral suspension
Equaline Children's Ibuprofen 100mg/5ml Suspension (Berry) (41163-0685) (Albertson's, Inc)
Ibuprofen Oral suspension
Equaline Children's Ibuprofen 100mg/5mL Suspension (Berry) (41163-0897) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral suspension
Equaline Children's Ibuprofen 100mg/5ml Suspension (Bubble Gum) (41163-0166) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral suspension
Equaline Children's Ibuprofen 100mg/5mL Suspension (Grape) (41163-0660) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral suspension
Equate Children's Ibuprofen 100mg/5ml Suspension (81131-0699) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
Equate Children's Ibuprofen 100mg/5mL Suspension (Berry) (49035-0897) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
Equate Children's Ibuprofen 100mg/5mL Suspension (Berry) (49035-0716) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
Equate Children's Ibuprofen 100mg/5mL Suspension (Berry) (49035-0693) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
Equate Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (49035-0166) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
Equate Children's Ibuprofen 8 Hour 100mg/5ml Suspension (Berry) (49035-0126) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
Equate Ibuprofen Children's 100mg/5ml Suspension (Berry) (49035-0660) (Wal-Mart Stores, Inc.)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Berry) (24385-0905) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Berry) (24385-0009) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Berry) (24385-0905) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Berry) (24385-0009) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (24385-0361) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (24385-0361) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (24385-0361) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Grape) (24385-0372) (AmerisourceBergen Corporation) (2024-09-24T00:00:00)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Grape) (46122-0110) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Grape) (24385-0372) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GNP Children's Ibuprofen 100mg/5mL Suspension (Grape) (24385-0372) (AmerisourceBergen Corporation)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Berry) (00113-0897) (Goodsense a Division of Perrigo)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Berry) (00113-0685) (Goodsense a Division of Perrigo)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (00113-0166) (Goodsense a Division of Perrigo) (2012-10-08T00:00:00)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (00113-0166) (Goodsense a Division of Perrigo)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Fruit) (00113-0623) (Goodsense a Division of Perrigo)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Grape) (00113-0660) (Goodsense a Division of Perrigo) (2012-09-11T00:00:00)
Ibuprofen Oral suspension
GoodSense Children's Ibuprofen 100mg/5mL Suspension (Grape) (00113-0660) (Goodsense a Division of Perrigo)
Ibuprofen Oral suspension
Health Mart Children's Ibuprofen 100mg/5mL Suspension (Berry) (62011-0030) (McKesson Corporation) (2023-03-30T00:00:00)
Ibuprofen Oral suspension
Health Mart Children's Ibuprofen 100mg/5mL Suspension (Berry) (62011-0214) (McKesson Corporation) (2022-07-27T00:00:00)
Ibuprofen Oral suspension
Health Mart Children's Ibuprofen 100mg/5mL Suspension (Berry) (62011-0030) (McKesson Corporation)
Ibuprofen Oral suspension
Health Mart Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (62011-0011) (McKesson Corporation) (2022-07-27T00:00:00)
Ibuprofen Oral suspension
Health Mart Children's Ibuprofen 100mg/5mL Suspension (Grape) (62011-0010) (McKesson Corporation) (2022-07-27T00:00:00)
Ibuprofen Oral suspension
HEB Ibuprofen Children's 100mg/5ml Suspension (Berry) (37808-0897) (H-E-B)
Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (45802-0952) (Padagis US LLC)

Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (45802-0952) (Padagis US LLC)

Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (10768-7019) (Perrigo Rx)

Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (00121-4774) (Pharmaceutical Associates Inc.) (2012-07-05T00:00:00)
Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (00472-1270) (Teva/Actavis US) (2007-01-16T00:00:00)

Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (66689-0009) (Vistapharm Inc) (2019-03-28T00:00:00)
Ibuprofen Oral suspension
Ibuprofen 100mg/5ml Suspension (50962-0475) (Xactdose Inc.) (2005-04-26T00:00:00)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (59651-0032) (Aurobindo Pharma Limited)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (50383-0584) (Hi-Tech Pharmacal, a subsidiary of Akorn) (2019-12-01T00:00:00)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (50383-0584) (Hi-Tech Pharmacal, a subsidiary of Akorn) (2019-08-20T00:00:00)
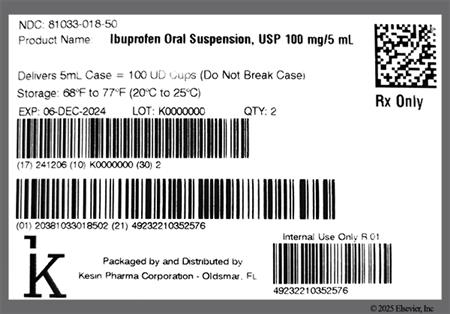
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (81033-0018) (Kesin Pharma Corporation)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (00121-4774) (Pharmaceutical Associates Inc.) (2025-08-01T00:00:00)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (00121-0918) (Pharmaceutical Associates Inc.) (2024-01-30T00:00:00)
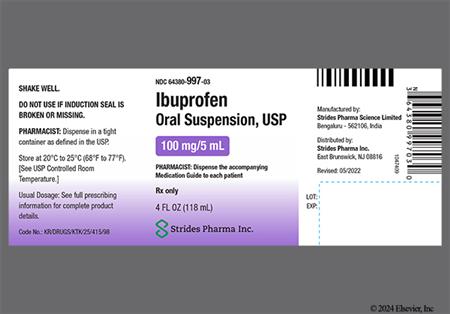
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (64380-0997) (Strides Pharma Science Limited)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (51672-1385) (Taro Pharmaceuticals USA Inc)

Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (51672-1409) (Taro Pharmaceuticals USA Inc)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (51672-2138) (Taro Pharmaceuticals USA Inc)
Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (00472-1270) (Teva/Actavis US) (2018-08-08T00:00:00)

Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (00472-2002) (Teva/Actavis US)

Ibuprofen Oral suspension
Ibuprofen 100mg/5mL Suspension (66689-0339) (Vistapharm Inc) (2022-08-29T00:00:00)
Ibuprofen Oral suspension
Kroger Children's Ibuprofen 100mg/5mL Suspension (Berry) (30142-0897) (The Kroger Co.)
Ibuprofen Oral suspension
Kroger Children's Ibuprofen 100mg/5ml Suspension (Bubble Gum) (30142-0166) (The Kroger Co.)
Ibuprofen Oral suspension
Kroger Children's Ibuprofen 100mg/5mL Suspension (Grape) (30142-0660) (The Kroger Co.)
Ibuprofen Oral suspension
Leader Children's Dye-Free Ibuprofen 100mg/5mL Suspension (Berry) (70000-0262) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5ml Suspension (Berry) (37205-0643) (Cardinal Health, Inc.) (2018-02-06T00:00:00)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Berry) (37205-0848) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Berry) (70000-0263) (Cardinal Health, Inc.) (2019-03-01T00:00:00)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Berry) (70000-0263) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Blue Raspberry) (70000-0259) (Cardinal Health, Inc.) (2022-09-13T00:00:00)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5ml Suspension (Bubblegum) (37205-0282) (Cardinal Health, Inc.) (2018-02-06T00:00:00)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (70000-0264) (Cardinal Health, Inc.) (2019-03-01T00:00:00)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (70000-0264) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Fruit) (37205-0644) (Cardinal Health, Inc.) (2005-01-28T00:00:00)

Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5ml Suspension (Grape) (37205-0283) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Grape) (37205-0660) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Grape) (70000-0181) (Cardinal Health, Inc.) (2019-03-01T00:00:00)
Ibuprofen Oral suspension
Leader Children's Ibuprofen 100mg/5mL Suspension (Grape) (70000-0181) (Cardinal Health, Inc.)
Ibuprofen Oral suspension
Motrin 100mg/5mL Suspension (50580-0448) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division) (2005-01-28T00:00:00)
Ibuprofen Oral suspension
Motrin 100mg/5mL Suspension (00045-0448) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2005-04-01T00:00:00)
Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Berry) (50580-0184) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division) (2012-07-23T00:00:00)
Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Berry) (00045-0192) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2012-07-09T00:00:00)

Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Berry) (50580-0184) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Berry) (50580-0184) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral suspension
Motrin Children's 100mg/5mL Suspension (Berry) (50580-0601) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Bubblegum) (00045-0604) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Grape) (50580-0603) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral suspension
Motrin Children's 100mg/5ml Suspension (Tropical Punch) (00045-0215) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2010-07-01T00:00:00)
Ibuprofen Oral suspension
PediaCare Children's Pain Reliever/Fever Reducer IB 100mg/5ml Suspension (Berry) (null) (Medtech Products, Inc., a subsidiary of Prestige Consumer Healthcare) (2018-12-31T00:00:00)
Ibuprofen Oral suspension
Premier Value Children's Ibuprofen 100mg/5mL Suspension (Berry) (68016-0255) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral suspension
Premier Value Children's Ibuprofen 100mg/5mL Suspension (Berry) (68016-0261) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral suspension
Premier Value Children's Ibuprofen 100mg/5mL Suspension (Berry) (68016-0250) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral suspension
Premier Value Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (68016-0263) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral suspension
Premier Value Children's Ibuprofen 100mg/5mL Suspension (Grape) (68016-0262) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral suspension
Publix Children's Profen IB 100mg/5ml Suspension (Berry) (56062-0897) (Publix Super Markets, Inc)
Ibuprofen Oral suspension
Publix Children's Profen IB 100mg/5ml Suspension (Bubblegum) (56062-0166) (Publix Super Markets, Inc)
Ibuprofen Oral suspension
Quality Choice Children's Ibuprofen 100mg/5mL Suspension (Berry) (63868-0756) (Chain Drug Marketing Association)
Ibuprofen Oral suspension
Quality Choice Children's Ibuprofen 100mg/5mL Suspension (Berry) (63868-0795) (Chain Drug Marketing Association)
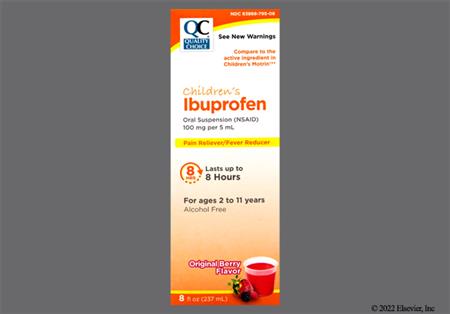
Ibuprofen Oral suspension
Quality Choice Children's Ibuprofen 100mg/5mL Suspension (Berry) (63868-0779) (Chain Drug Marketing Association)
Ibuprofen Oral suspension
Quality Choice Children's Ibuprofen 100mg/5mL Suspension (Bubble Gum) (63868-0758) (Chain Drug Marketing Association)
Ibuprofen Oral suspension
Quality Choice Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (63868-0796) (Chain Drug Marketing Association)
Ibuprofen Oral suspension
RITE AID Children's Ibuprofen 100mg/5mL Suspension (11822-0729) (Rite Aid Corp)
Ibuprofen Oral suspension
RITE AID Children's Ibuprofen 100mg/5mL Suspension (Berry) (null) (Rite Aid Corp)

Ibuprofen Oral suspension
RITE AID Children's Ibuprofen 100mg/5mL Suspension (Berry) (null) (Rite Aid Corp)

Ibuprofen Oral suspension
RITE AID Children's Ibuprofen 100mg/5mL Suspension (Berry) (null) (Rite Aid Corp)

Ibuprofen Oral suspension
RITE AID Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (null) (Rite Aid Corp)

Ibuprofen Oral suspension
RITE AID Children's Ibuprofen 100mg/5mL Suspension (Grape) (null) (Rite Aid Corp)

Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5ml Suspension (Berry) (70677-0150) (McKesson Corporation) (2023-12-31T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Berry) (49348-0229) (McKesson Corporation) (2023-06-15T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Berry) (49348-0876) (McKesson Corporation) (2023-06-15T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Berry) (70677-0151) (McKesson Corporation) (2023-09-25T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Bubble-Gum) (49348-0500) (McKesson Corporation) (2022-07-06T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Bubblegum) (70677-0152) (McKesson Corporation) (2023-11-05T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Grape) (49348-0499) (McKesson Corporation) (2023-06-15T00:00:00)
Ibuprofen Oral suspension
Sunmark Children's Ibuprofen 100mg/5mL Suspension (Grape) (70677-0153) (McKesson Corporation) (2023-11-05T00:00:00)
Ibuprofen Oral suspension
Top Care Children's Ibuprofen 100mg/5ml Suspension (Berry) (null) (Topco Associates LLC)
Ibuprofen Oral suspension
Top Care Children's Ibuprofen 100mg/5mL Suspension (Berry) (36800-0897) (Topco Associates LLC)
Ibuprofen Oral suspension
Top Care Children's Ibuprofen 100mg/5ml Suspension (Bubblegum) (36800-0166) (Topco Associates LLC)
Ibuprofen Oral suspension
Top Care Children's Ibuprofen 100mg/5mL Suspension (Grape) (36800-0660) (Topco Associates LLC)
Ibuprofen Oral suspension
up & up Children's Ibuprofen 100mg/5mL Suspension (Grape) (11673-0660) (Perrigo Company)
Ibuprofen Oral suspension
Walgreens Children's Dye-Free Ibuprofen 100mg/5mL Suspension (Berry) (00363-0806) (Walgreens Co.)
Ibuprofen Oral suspension
Walgreens Children's Dye-Free Ibuprofen 100mg/5mL Suspension (Berry) (00363-0806) (Walgreens Co.)

Ibuprofen Oral suspension
Walgreens Children's Ibuprofen 100mg/5ml Suspension (Berry) (11917-0005) (Walgreens Co.) (2013-08-07T00:00:00)
Ibuprofen Oral suspension
Walgreens Children's Ibuprofen 100mg/5mL Suspension (Berry) (00363-0897) (Walgreens Co.)
Ibuprofen Oral suspension
Walgreens Children's Ibuprofen 100mg/5mL Suspension (Bubble Gum) (00363-0166) (Walgreens Co.)

Ibuprofen Oral suspension
Walgreens Children's Ibuprofen 100mg/5mL Suspension (Grape) (00363-0660) (Walgreens Co.)

Ibuprofen Oral suspension
Ibuprofen 200mg/10mL Suspension (81033-0018) (Kesin Pharma Corporation)
Ibuprofen Oral tablet
Advil Junior Strength 100mg Tablet (00573-0175) (GlaxoSmithKline Consumer Healthcare) (2020-06-30T00:00:00)
Ibuprofen Oral tablet
Advil Junior Strength 100mg Tablet (00573-0175) (GlaxoSmithKline Consumer Healthcare) (2020-06-30T00:00:00)
Ibuprofen Oral tablet
Motrin Junior 100mg Caplet (00045-0498) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2012-06-01T00:00:00)
Ibuprofen Oral tablet
Advil 200mg Caplet (00573-0160) (Haleon US Holdings LLC)
Ibuprofen Oral tablet
Advil 200mg Caplet (00573-0161) (Haleon US Holdings LLC)
Ibuprofen Oral tablet
Advil 200mg Gel Caplet (00573-0165) (GlaxoSmithKline Consumer Healthcare)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0151) (GlaxoSmithKline Consumer Healthcare) (2011-10-01T00:00:00)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0152) (GlaxoSmithKline Consumer Healthcare) (2008-04-29T00:00:00)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0154) (GlaxoSmithKline Consumer Healthcare) (2008-04-29T00:00:00)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0162) (GlaxoSmithKline Consumer Healthcare) (2020-06-30T00:00:00)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0154) (GlaxoSmithKline Consumer Healthcare)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0133) (GlaxoSmithKline Consumer Healthcare)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0134) (GlaxoSmithKline Consumer Healthcare)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0150) (Haleon US Holdings LLC)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0151) (Haleon US Holdings LLC)
Ibuprofen Oral tablet
Advil 200mg Tablet (00573-0154) (Haleon US Holdings LLC)
Ibuprofen Oral tablet
CAREALL Ibuprofen 200mg Tablet (51824-0064) (New World Imports Inc)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0292) (CVS Health) (2018-02-28T00:00:00)

Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (null) (CVS Health) (2016-03-31T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0292) (CVS Health) (2018-10-31T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0292) (CVS Health) (2017-09-30T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0292) (CVS Health) (2018-08-31T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0292) (CVS Health) (2018-08-31T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0393) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0647) (CVS Health)

Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0647) (CVS Health)

Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (59779-0647) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Caplet (69842-0183) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0291) (CVS Health)

Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health) (2017-08-31T00:00:00)

Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health) (2017-08-31T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0291) (CVS Health) (2018-04-30T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health) (2018-02-28T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0074) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0604) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0392) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0604) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0604) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0291) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen 200mg Tablet (59779-0291) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen Dye-Free 200mg Tablet (59779-0438) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen Dye-Free 200mg Tablet (null) (CVS Health)
Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Caplet (59779-0393) (CVS Health) (2016-03-30T00:00:00)

Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Caplet (null) (CVS Health) (2018-10-31T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Caplet (59779-0393) (CVS Health) (2017-03-22T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Caplet (59779-0517) (CVS Health)

Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Tablet (59779-0392) (CVS Health)

Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Tablet (null) (CVS Health) (2017-03-21T00:00:00)
Ibuprofen Oral tablet
CVS Ibuprofen IB 200mg Tablet (59779-0392) (CVS Health)
Ibuprofen Oral tablet
Dover Addaprin 200mg Tablet (47682-0614) (UniFirst First-Aid Corporation)
Ibuprofen Oral tablet
Equaline Ibuprofen 200mg Caplet (41163-0297) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Equaline Ibuprofen 200mg Tablet (41163-0604) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Equaline Ibuprofen 200mg Tablet (41163-0647) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Equaline Ibuprofen 200mg Tablet (41163-0114) (Albertson's, Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Equaline Ibuprofen 200mg Tablet (41163-0604) (Albertson's, Inc)
Ibuprofen Oral tablet
Equate Ibuprofen 200mg Tablet (49035-0604) (Wal-Mart Stores, Inc.)
Ibuprofen Oral tablet
Equate Ibuprofen 200mg Tablet (49035-0912) (Wal-Mart Stores, Inc.)
Ibuprofen Oral tablet
Equate Ibuprofen 200mg Tablet (49035-0438) (Wal-Mart Stores, Inc.)
Ibuprofen Oral tablet
Equate Ibuprofen 200mg Tablet (49035-0647) (Wal-Mart Stores, Inc.)
Ibuprofen Oral tablet
Equate Ibuprofen 200mg Tablet (49035-0517) (Wal-Mart Stores, Inc.)
Ibuprofen Oral tablet
Equate Ibuprofen 200mg Tablet (49035-0553) (Wal-Mart Stores, Inc.)
Ibuprofen Oral tablet
Foster & Thrive Ibuprofen 200mg Caplet (70677-1136) (McKesson Corporation)
Ibuprofen Oral tablet
Foster & Thrive Ibuprofen 200mg Tablet (70677-1132) (McKesson Corporation)

Ibuprofen Oral tablet
Foster & Thrive Pain Relief 200mg Tablet (70677-1244) (McKesson Corporation)

Ibuprofen Oral tablet
Genpril 200mg Tablet (00182-2401) (Teva Pharmaceuticals USA)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Caplet (24385-0058) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Caplet (24385-0647) (AmerisourceBergen Corporation)

Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (24385-0604) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (24385-0647) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (24385-0059) (AmerisourceBergen Corporation) (2024-01-31T00:00:00)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (46122-0341) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (24385-0604) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (46122-0227) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (24385-0604) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (46122-0548) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GNP Ibuprofen 200mg Tablet (null) (AmerisourceBergen Corporation)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Caplet (00113-0647) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Caplet (00113-0517) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Tablet (00113-0669) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Tablet (00113-0995) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Tablet (00113-0604) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Tablet (00113-0628) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Tablet (00113-0074) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
GoodSense Ibuprofen 200mg Tablet (00113-1212) (Goodsense a Division of Perrigo)
Ibuprofen Oral tablet
Health Mart Ibuprofen 200mg Caplet (62011-0015) (McKesson Corporation) (2022-11-18T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen 200mg Caplet (62011-0015) (McKesson Corporation) (2020-12-18T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen 200mg Tablet (62011-0013) (McKesson Corporation) (2012-08-14T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen 200mg Tablet (62011-0014) (McKesson Corporation) (2023-02-09T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen 200mg Tablet (62011-0039) (McKesson Corporation) (2012-11-30T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen 200mg Tablet (62011-0014) (McKesson Corporation) (2023-06-23T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen IB 200mg Caplet (62011-0213) (McKesson Corporation) (2021-02-25T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen IB 200mg Tablet (62011-0222) (McKesson Corporation) (2022-11-18T00:00:00)
Ibuprofen Oral tablet
Health Mart Ibuprofen IB 200mg Tablet (62011-0222) (McKesson Corporation) (2022-11-18T00:00:00)
Ibuprofen Oral tablet
Henry Schein Ibuprofen 200mg Tablet (00404-0017) (Henry Schein Inc.)
Ibuprofen Oral tablet
I-PRIN 200mg Tablet (47682-0100) (UniFirst First-Aid Corporation)
Ibuprofen Oral tablet
Ibu-200 200mg Tablet (00904-1747) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2009-09-29T00:00:00)
Ibuprofen Oral tablet
Ibu-200 200mg Tablet (00904-7914) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2020-06-11T00:00:00)
Ibuprofen Oral tablet
Ibu-Tab 200mg Tablet (51641-0215) (Alra Laboratories Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Caplet (00904-7912) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 200mg Caplet (68788-8148) (Preferred Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 200mg Caplet (00536-1089) (Rugby Laboratories a Division of The Harvard Drug Group, LLC)
Ibuprofen Oral tablet
Ibuprofen 200mg Caplet (66424-0396) (SDA Laboratories, Inc.)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (50090-5223) (A-S Medication Solutions LLC)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (65162-0565) (Akyma Pharmaceuticals, a subsidiary of Amneal Pharmaceuticals) (2008-02-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (65162-0565) (Amneal Pharmaceuticals LLC) (2008-08-29T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (53746-0140) (Amneal Pharmaceuticals LLC) (2019-07-17T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00304-1710) (Balan, J.J. Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00761-0908) (Basic Drugs Inc)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (61919-0123) (Direct Rx)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (52735-0732) (Family Pharmacy)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (52735-0750) (Family Pharmacy)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (52735-0751) (Family Pharmacy)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (52735-0758) (Family Pharmacy)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (57896-0941) (Geri-Care Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (57896-0540) (Geri-Care Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (57896-0941) (Geri-Care Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (54162-0941) (Geritrex Corporation)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (53746-0135) (Interpharm Inc)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (52189-0221) (Invamed Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00820-0133) (Logen Pharmaceuticals Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-5323) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2014-01-06T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-7914) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-7915) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2009-12-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-7914) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2010-11-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-7915) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2019-01-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-7915) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2019-09-26T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-7914) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)

Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00904-6747) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (10135-0183) (Marlex Pharmaceuticals) (2014-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (10135-0290) (Marlex Pharmaceuticals) (2016-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (10135-0143) (Marlex Pharmaceuticals) (2016-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (null) (Mason Vitamins)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (null) (Mason Vitamins)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (null) (Mason Vitamins)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (null) (Mason Vitamins)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (49348-0706) (McKesson Corporation)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (49348-0808) (McKesson Corporation)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (49348-0809) (McKesson Corporation)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (63739-0134) (McKesson Packaging Inc) (2006-01-27T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (51079-0731) (Mylan Institutional LLC) (2010-06-07T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (54629-0905) (National Vitamin Company Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (54629-0960) (National Vitamin Company Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (54629-0961) (National Vitamin Company Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00084-0052) (Natural Nutritionals Company) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00084-0054) (Natural Nutritionals Company) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (66267-0115) (NuCare Pharmaceuticals Inc) (2008-04-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (55289-0673) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (43063-0890) (PD-Rx Pharmaceuticals, Inc.) (2020-02-25T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (72789-0191) (PD-Rx Pharmaceuticals, Inc.)
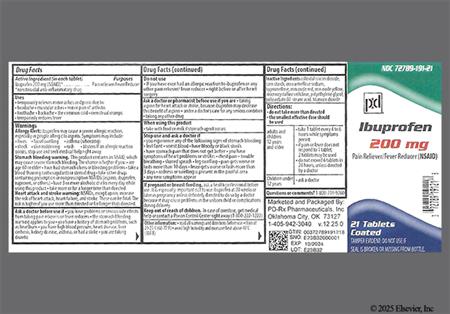
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (16103-0393) (Pharbest Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (16103-0407) (Pharbest Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (52605-0114) (Polygen Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (17236-0565) (R&S Northeast, LLC, formerly Dixon-Shane Drug Company) (2005-05-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (10956-0678) (Reese Pharmaceutical Company)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (10956-0679) (Reese Pharmaceutical Company)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00122-0808) (Rexall Group) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00122-0847) (Rexall Group) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00122-0881) (Rexall Group) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (60814-0127) (Rexall Group) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (60814-0128) (Rexall Group) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-3939) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2008-11-20T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-3105) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2011-08-10T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-3105) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2012-07-11T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-3587) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2013-03-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-3587) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2014-11-06T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-1088) (Rugby Laboratories a Division of The Harvard Drug Group, LLC) (2019-03-29T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00536-1390) (Rugby Laboratories a Division of The Harvard Drug Group, LLC ) (2025-04-29T00:00:00)

Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00781-1349) (Sandoz Inc. a Novartis Company) (2005-05-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (60760-0941) (St. Mary's Medical Park Pharmacy)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00677-1090) (Sun Pharmaceutical Industries, Inc.) (2005-11-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00677-1947) (Sun Pharmaceutical Industries, Inc.) (2007-10-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00093-0483) (Teva Pharmaceuticals USA) (2005-04-22T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00093-0486) (Teva Pharmaceuticals USA) (2005-04-22T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00182-1039) (Teva Pharmaceuticals USA) (2010-02-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (50732-0133) (Teva Pharmaceuticals USA) (2005-05-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00182-8688) (Teva Pharmaceuticals USA) (2010-01-07T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (00364-2145) (Teva/Actavis US) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (49483-0601) (Time Cap Laboratories Inc)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (47682-0100) (UniFirst First-Aid Corporation)
Ibuprofen Oral tablet
Ibuprofen 200mg Tablet (11383-0068) (Weeks and Leo)
Ibuprofen Oral tablet
Kirkland Ibuprofen 200mg Caplet (63981-0393) (Costco Wholesale Corporation)
Ibuprofen Oral tablet
Kirkland Ibuprofen 200mg Tablet (63981-0604) (Costco Wholesale Corporation)
Ibuprofen Oral tablet
Kirkland Ibuprofen 200mg Tablet (63981-0291) (Costco Wholesale Corporation)
Ibuprofen Oral tablet
Kroger Ibuprofen 200mg Caplet (30142-0517) (The Kroger Co.)
Ibuprofen Oral tablet
Kroger Ibuprofen 200mg Caplet (30142-0647) (The Kroger Co.)
Ibuprofen Oral tablet
Kroger Ibuprofen 200mg Tablet (30142-0604) (The Kroger Co.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (37205-0341) (Cardinal Health, Inc.) (2014-10-28T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (37205-0605) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0176) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0176) (Cardinal Health, Inc.) (2019-03-01T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0175) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0176) (Cardinal Health, Inc.) (2020-10-08T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0288) (Cardinal Health, Inc.) (2021-04-29T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0176) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Caplet (70000-0003) (Cardinal Health, Inc.) (2024-01-08T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0175) (Cardinal Health Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (37205-0345) (Cardinal Health, Inc.) (2017-11-07T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (37205-0350) (Cardinal Health, Inc.) (2014-10-28T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0308) (Cardinal Health, Inc.) (2022-10-12T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0175) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0175) (Cardinal Health, Inc.) (2019-03-01T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0291) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0308) (Cardinal Health, Inc.) (2022-10-12T00:00:00)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0003) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0175) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0292) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Leader Ibuprofen 200mg Tablet (70000-0597) (Cardinal Health, Inc.)
Ibuprofen Oral tablet
Midol Cramps and Body Aches Formula 200mg Tablet (12843-0143) (Bayer Corp Consumer Care Div) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Motrin IB 200mg Caplet (00045-0481) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2018-05-31T00:00:00)
Ibuprofen Oral tablet
Motrin IB 200mg Caplet (00045-0481) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2016-11-14T00:00:00)
Ibuprofen Oral tablet
Motrin IB 200mg Caplet (50580-0230) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.)
Ibuprofen Oral tablet
Motrin IB 200mg Tablet (00045-0463) (McNeil Consumer Healthcare Division of McNEIL-PPC, Inc.) (2013-01-21T00:00:00)
Ibuprofen Oral tablet
Motrin Migraine Pain 200mg Caplet (50580-0119) (Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division) (2005-08-02T00:00:00)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Caplet (68016-0004) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Caplet (68016-0004) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Caplet (68016-0645) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0059) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0024) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0030) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0295) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0030) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0634) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0635) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Premier Value Ibuprofen 200mg Tablet (68016-0634) (Pharmacy Value Alliance LLC formerly Chain Drug Consortium , LLC)
Ibuprofen Oral tablet
Publix Ibuprofen 200mg Tablet (56062-0604) (Publix Super Markets, Inc)
Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Caplet (63868-0979) (Chain Drug Marketing Association)

Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Caplet (63868-0570) (Chain Drug Marketing Association) (2025-06-09T00:00:00)
Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Caplet (83324-0100) (Chain Drug Marketing Association)
Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Tablet (63868-0773) (Chain Drug Marketing Association)

Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Tablet (63868-0571) (Chain Drug Marketing Association) (2025-06-09T00:00:00)
Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Tablet (63868-0268) (Chain Drug Marketing Association)
Ibuprofen Oral tablet
Quality Choice Ibuprofen 200mg Tablet (83324-0102) (Chain Drug Marketing Association)
Ibuprofen Oral tablet
Quality Choice Ibuprofen IB 200mg Caplet (63868-0791) (Chain Drug Marketing Association) (2025-06-09T00:00:00)
Ibuprofen Oral tablet
Quality Choice Ibuprofen IB 200mg Tablet (63868-0790) (Chain Drug Marketing Association) (2025-06-09T00:00:00)
Ibuprofen Oral tablet
Quality Choice Ibuprofen IB 200mg Tablet (63868-0794) (Chain Drug Marketing Association) (2025-06-09T00:00:00)
Ibuprofen Oral tablet
RITE AID Ibuprofen 200mg Caplet (11822-0790) (Rite Aid Corp)
Ibuprofen Oral tablet
RITE AID Ibuprofen 200mg Tablet (null) (Rite Aid Corp)
Ibuprofen Oral tablet
RITE AID Ibuprofen 200mg Tablet (11822-0032) (Rite Aid Corp)
Ibuprofen Oral tablet
RITE AID Ibuprofen 200mg Tablet (11822-0305) (Rite Aid Corp)
Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Caplet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Caplet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Caplet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Caplet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
RITE AID Ibuprofen Pain Relief 200mg Tablet (null) (Rite Aid Corp)

Ibuprofen Oral tablet
Select Brand Ibuprofen 200mg Caplet (15127-0335) (Select Brand)

Ibuprofen Oral tablet
Select Brand Ibuprofen 200mg Caplet (15127-0907) (Select Brand)
Ibuprofen Oral tablet
Select Brand Ibuprofen 200mg Tablet (15127-0312) (Select Brand)

Ibuprofen Oral tablet
Select Brand Ibuprofen 200mg Tablet (15127-0905) (Select Brand)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Caplet (10939-0356) (McKesson Corporation) (2023-11-22T00:00:00)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0196) (McKesson Corporation)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0706) (McKesson Corporation) (2024-01-23T00:00:00)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0706) (McKesson Corporation) (2024-09-15T00:00:00)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0706) (McKesson Corporation) (2024-01-30T00:00:00)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0706) (McKesson Corporation) (2024-02-10T00:00:00)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0706) (McKesson Corporation) (2024-08-16T00:00:00)
Ibuprofen Oral tablet
Sunmark Ibuprofen 200mg Tablet (49348-0927) (McKesson Corporation)
Ibuprofen Oral tablet
Sunmark Ibuprofen IB 200mg Caplet (49348-0727) (McKesson Corporation)
Ibuprofen Oral tablet
Today's Health Ibuprofen 200mg Caplet (null) (Today's Health, Inc.)
Ibuprofen Oral tablet
Today's Health Ibuprofen 200mg Tablet (null) (Today's Health, Inc.)
Ibuprofen Oral tablet
Today's Health Ibuprofen 200mg Tablet (null) (Today's Health, Inc.)
Ibuprofen Oral tablet
Top Care Ibuprofen 200mg Caplet (36800-0183) (Topco Associates LLC)
Ibuprofen Oral tablet
Top Care Ibuprofen 200mg Caplet (36800-0517) (Topco Associates LLC)
Ibuprofen Oral tablet
Top Care Ibuprofen 200mg Caplet (36800-0647) (Topco Associates LLC)
Ibuprofen Oral tablet
Top Care Ibuprofen 200mg Tablet (36800-0144) (Topco Associates LLC)
Ibuprofen Oral tablet
Top Care Ibuprofen 200mg Tablet (36800-0074) (Topco Associates LLC)
Ibuprofen Oral tablet
Wal-Profen 200mg Caplet (00363-0292) (Walgreens Co.) (2007-03-12T00:00:00)
Ibuprofen Oral tablet
Wal-Profen 200mg Caplet (00363-0292) (Walgreens Co.) (2007-03-12T00:00:00)
Ibuprofen Oral tablet
Wal-Profen 200mg Tablet (11917-0043) (Walgreens Co.)
Ibuprofen Oral tablet
Wal-Profen 200mg Tablet (00363-0291) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Caplet (00363-0393) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Caplet (00363-0292) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Caplet (00363-0393) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Caplet (11917-0049) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Caplet (00363-0705) (Walgreens Co.)

Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Caplet (00363-1517) (Walgreens Co.)

Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0392) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0438) (Walgreens Co.)

Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0910) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0392) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0392) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (11917-0056) (Walgreens Co.)

Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0291) (Walgreens Co.)
Ibuprofen Oral tablet
Walgreens Ibuprofen 200mg Tablet (00363-0909) (Walgreens Co.)
Ibuprofen Oral tablet
Ibuprofen 300mg Tablet (70512-0794) (Sola Pharmaceuticals)
Ibuprofen Oral tablet
IBU 400mg Tablet (67877-0119) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2014-01-01T00:00:00)
Ibuprofen Oral tablet
IBU 400mg Tablet (49884-0467) (Endo USA, Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
IBU 400mg Tablet (49884-0777) (Endo USA, Inc.) (2011-03-02T00:00:00)
Ibuprofen Oral tablet
Ibu-Tab 400mg Tablet (51641-0214) (Alra Laboratories Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (50090-6676) (A-S Medication Solutions LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (50090-6677) (A-S Medication Solutions LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (50090-5160) (A-S Medication Solutions LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (11788-0008) (AiPing Pharmaceutical, Inc.) (2023-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (11788-0008) (AiPing Pharmaceutical, Inc.)

Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (65162-0568) (Akyma Pharmaceuticals, a subsidiary of Amneal Pharmaceuticals) (2008-02-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (69512-0400) (Alivio Medical Products)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (62584-0746) (American Health Packaging) (2013-09-20T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (68084-0658) (American Health Packaging) (2019-09-29T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (60687-0446) (American Health Packaging)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (65162-0568) (Amneal Pharmaceuticals LLC) (2008-08-29T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (53746-0131) (Amneal Pharmaceuticals LLC) (2010-01-21T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (53746-0464) (Amneal Pharmaceuticals LLC) (2019-12-17T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (65162-1101) (Amneal Pharmaceuticals LLC) (2015-03-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (69238-1101) (Amneal Pharmaceuticals LLC) (2019-02-26T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (65162-0464) (Amneal Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (43353-0389) (Aphena Pharma Solutions - Tennessee, LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (67877-0119) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2012-02-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (67877-0119) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2015-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (67877-0294) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (67877-0319) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (59651-0360) (Aurobindo Pharma Limited)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (42291-0337) (AvKARE, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (42291-0440) (AvKARE, Inc.) (2024-09-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (42582-0111) (Bi-Coastal Pharmaceutical Corp.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (10544-0625) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (10544-0030) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (10544-0213) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (10544-0201) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (51991-0720) (Breckenridge Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (53403-0537) (BV Pharbita) (2005-04-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (62135-0400) (Chartwell RX LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (55111-0101) (Dr. Reddy's Laboratories, Inc.) (2008-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (55111-0682) (Dr. Reddy's Laboratories, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (51293-0843) (ECI Pharmaceuticals )
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (49884-0162) (Endo USA, Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (76282-0712) (Exelan Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (71921-0180) (Florida Pharmaceutical Products, LLC.)

Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (60429-0219) (Golden State Medical Supply, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (51407-0369) (Golden State Medical Supply, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (51407-0839) (Golden State Medical Supply, Inc.)

Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (52959-0075) (HJ Harkins Co Inc)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00839-7112) (HL Moore Drug Exchange) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (61808-0230) (Imiren Pharmaceuticals Inc) (2004-05-14T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (50742-0157) (Ingenus Pharmaceuticals, LLC) (2015-11-02T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (53746-0131) (Interpharm Inc) (2008-06-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (68645-0220) (Legacy Pharmaceutical Packaging, LLC) (2017-04-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (68645-0474) (Legacy Pharmaceutical Packaging, LLC) (2017-04-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (68645-0529) (Legacy Pharmaceutical Packaging, LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (68645-0561) (Legacy Pharmaceutical Packaging, LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00904-1748) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2013-10-22T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00904-5185) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2006-01-13T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00904-5853) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00904-5853) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)

Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (63739-0672) (McKesson Packaging) (2020-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (63739-0135) (McKesson Packaging Inc) (2011-03-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (63739-0442) (McKesson Packaging Inc) (2015-07-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (58657-0680) (Method Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (51079-0281) (Mylan Institutional LLC) (2009-10-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (59762-7378) (Mylan Pharmaceutiacals, Inc.) (2006-09-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00378-0401) (Mylan Pharmaceuticals Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00378-1401) (Mylan Pharmaceuticals Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (66267-0116) (NuCare Pharmaceuticals Inc) (2008-04-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00603-4018) (Par Health USA, LLC) (2009-07-02T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00603-4021) (Par Health USA, LLC) (2010-10-26T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (55289-0590) (PD-Rx Pharmaceuticals, Inc.) (2011-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (43063-0308) (PD-Rx Pharmaceuticals, Inc.) (2019-06-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (55289-0590) (PD-Rx Pharmaceuticals, Inc.) (2015-06-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (43063-0843) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (43063-0872) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (43063-0872) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (72789-0185) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (72789-0201) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (45802-0184) (Perrigo Pharmaceuticals Company) (2008-08-14T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (10768-7373) (Perrigo Rx) (2008-02-06T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (52605-0121) (Polygen Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (17236-0568) (R&S Northeast, LLC, formerly Dixon-Shane Drug Company) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00781-1352) (Sandoz, Inc. a Novartis Company) (2005-04-25T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00364-0765) (Schein Pharmaceutical Inc, an Actavis Company) (2005-04-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (73086-0210) (Skya Health, LLC)

Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (70436-0180) (Slate Run Pharmaceuticals, LLC)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (42543-0966) (Strides Pharma Inc)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (64380-0809) (Strides Pharma Science Limited)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00677-1031) (Sun Pharmaceutical Industries, Inc.) (2008-04-25T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00182-1809) (Teva Pharmaceuticals USA) (2009-08-13T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (50111-0387) (Teva Pharmaceuticals USA) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00172-4018) (Teva Pharmaceuticals USA) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00591-4010) (Teva/Actavis US) (2005-05-25T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00591-3464) (Teva/Actavis US) (2008-11-12T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (00591-3663) (Teva/Actavis US) (2009-10-22T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (49483-0602) (Time Cap Laboratories Inc)
Ibuprofen Oral tablet
Ibuprofen 400mg Tablet (69367-0394) (Westminster Pharmaceuticals, LLC)

Ibuprofen Oral tablet
Motrin 400mg Tablet (00009-7385) (Pfizer Inc.) (2006-12-11T00:00:00)
Ibuprofen Oral tablet
Ibren 600mg Tablet (38130-0053) (Emrex Economed Pharmaceuticals Inc)
Ibuprofen Oral tablet
IBU 600mg Tablet (67877-0120) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2014-01-01T00:00:00)
Ibuprofen Oral tablet
IBU 600mg Tablet (49884-0468) (Endo USA, Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
IBU 600mg Tablet (49884-0778) (Endo USA, Inc.) (2011-03-02T00:00:00)
Ibuprofen Oral tablet
Ibu-Tab 600mg Tablet (51641-0213) (Alra Laboratories Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibupak 600mg Kit (59088-0756) (PureTek Corporation)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (50090-2626) (A-S Medication Solutions LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (11788-0009) (AiPing Pharmaceutical, Inc.) (2023-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (11788-0009) (AiPing Pharmaceutical, Inc.)

Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (65162-0569) (Akyma Pharmaceuticals, a subsidiary of Amneal Pharmaceuticals) (2008-02-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (69512-0600) (Alivio Medical Products)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (62584-0747) (American Health Packaging) (2013-09-20T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (68084-0703) (American Health Packaging) (2019-05-26T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (60687-0457) (American Health Packaging)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (65162-0569) (Amneal Pharmaceuticals LLC) (2008-08-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (53746-0132) (Amneal Pharmaceuticals LLC) (2010-01-21T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (53746-0465) (Amneal Pharmaceuticals LLC) (2019-06-03T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (65162-1102) (Amneal Pharmaceuticals LLC) (2015-03-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (69238-1102) (Amneal Pharmaceuticals LLC) (2019-03-11T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (65162-0465) (Amneal Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (43353-0393) (Aphena Pharma Solutions - Tennessee, LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (67877-0120) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2012-02-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (67877-0120) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2015-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (67877-0295) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (67877-0320) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (59651-0361) (Aurobindo Pharma Limited)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (42291-0338) (AvKARE, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (42291-0441) (AvKARE, Inc.) (2024-09-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (42582-0112) (Bi-Coastal Pharmaceutical Corp.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (10544-0014) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (10544-0015) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (10544-0214) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (10544-0430) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (51991-0730) (Breckenridge Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (62135-0401) (Chartwell RX LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (55111-0102) (Dr. Reddy's Laboratories, Inc.) (2008-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (55111-0683) (Dr. Reddy's Laboratories, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (51293-0844) (ECI Pharmaceuticals )
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (49884-0163) (Endo USA, Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (76282-0713) (Exelan Pharmaceuticals, Inc.)

Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (71921-0181) (Florida Pharmaceutical Products, LLC.)

Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (60429-0220) (Golden State Medical Supply, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (51407-0370) (Golden State Medical Supply, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (51407-0840) (Golden State Medical Supply, Inc.)

Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (52959-0076) (HJ Harkins Co Inc)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (50742-0158) (Ingenus Pharmaceuticals, LLC) (2015-11-02T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (53746-0132) (Interpharm Inc) (2008-06-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (68645-0221) (Legacy Pharmaceutical Packaging, LLC) (2017-04-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (68645-0475) (Legacy Pharmaceutical Packaging, LLC) (2017-04-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (68645-0530) (Legacy Pharmaceutical Packaging, LLC) (2019-03-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (68645-0562) (Legacy Pharmaceutical Packaging, LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00904-5186) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2013-10-29T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00904-5854) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00904-5854) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2025-06-19T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (63739-0684) (McKesson Packaging) (2020-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (63739-0136) (McKesson Packaging Inc) (2010-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (63739-0443) (McKesson Packaging Inc) (2011-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (58657-0681) (Method Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (55370-0534) (Mova Pharmaceuticals Corp) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (51079-0282) (Mylan Institutional LLC) (2009-10-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (59762-7379) (Mylan Pharmaceutiacals, Inc.) (2006-09-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00378-0601) (Mylan Pharmaceuticals Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00378-1601) (Mylan Pharmaceuticals Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (66267-0117) (NuCare Pharmaceuticals Inc) (2008-04-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (66267-0964) (NuCare Pharmaceuticals Inc) (2008-04-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00603-4019) (Par Health USA, LLC) (2009-06-11T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00603-4022) (Par Health USA, LLC) (2011-05-03T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (55289-0142) (PD-Rx Pharmaceuticals, Inc.) (2010-09-16T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (43063-0352) (PD-Rx Pharmaceuticals, Inc.) (2025-11-10T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (55289-0412) (PD-Rx Pharmaceuticals, Inc.) (2018-10-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (55289-0142) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (43063-0845) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (43063-0867) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (43063-0936) (PD-Rx Pharmaceuticals, Inc.) (2025-11-13T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (72789-0187) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (72789-0212) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (72789-0363) (PD-Rx Pharmaceuticals, Inc.)
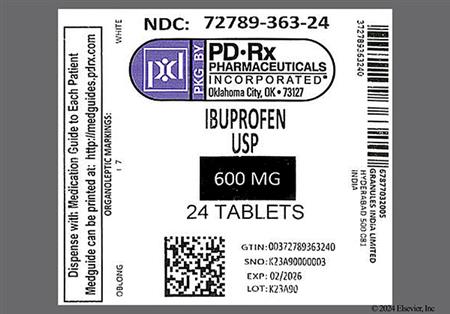
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (45802-0427) (Perrigo Pharmaceuticals Company) (2008-08-14T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (52605-0122) (Polygen Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (17236-0569) (R&S Northeast, LLC, formerly Dixon-Shane Drug Company) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (33358-0187) (RxChange Co.) (2024-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00781-1362) (Sandoz, Inc. a Novartis Company) (2005-04-25T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00364-0766) (Schein Pharmaceutical Inc, an Actavis Company) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (73086-0211) (Skya Health, LLC)

Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (70436-0181) (Slate Run Pharmaceuticals, LLC)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (42543-0965) (Strides Pharma Inc)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (64380-0808) (Strides Pharma Science Limited)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00677-1032) (Sun Pharmaceutical Industries, Inc.)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (50111-0388) (Teva Pharmaceuticals USA) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00172-3646) (Teva Pharmaceuticals USA) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00182-1810) (Teva Pharmaceuticals USA) (2009-12-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00591-4011) (Teva/Actavis US) (2006-03-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00591-3465) (Teva/Actavis US) (2009-02-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (00591-3664) (Teva/Actavis US) (2009-11-10T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (49483-0603) (Time Cap Laboratories Inc)
Ibuprofen Oral tablet
Ibuprofen 600mg Tablet (69367-0395) (Westminster Pharmaceuticals, LLC)

Ibuprofen Oral tablet
Motrin 600mg Tablet (00009-7386) (Pfizer Inc.) (2008-02-26T00:00:00)
Ibuprofen Oral tablet
Toxicology Saliva Collection Kit (69176-0035) (TMIG, Inc) (2024-12-31T00:00:00)
Ibuprofen Oral tablet
IBU 800mg Tablet (67877-0121) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2014-01-01T00:00:00)
Ibuprofen Oral tablet
IBU 800mg Tablet (49884-0469) (Endo USA, Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
IBU 800mg Tablet (49884-0779) (Endo USA, Inc.) (2011-03-02T00:00:00)
Ibuprofen Oral tablet
IBU 800mg Tablet (55289-0140) (PD-Rx Pharmaceuticals, Inc.) (2015-04-28T00:00:00)
Ibuprofen Oral tablet
Ibu-Tab 800mg Tablet (51641-0212) (Alra Laboratories Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (11788-0010) (AiPing Pharmaceutical, Inc.) (2023-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (11788-0010) (AiPing Pharmaceutical, Inc.)

Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (65162-0570) (Akyma Pharmaceuticals, a subsidiary of Amneal Pharmaceuticals) (2008-01-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (69512-0800) (Alivio Medical Products)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00047-0914) (Allergan USA, Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (62584-0748) (American Health Packaging) (2013-12-23T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (68084-0772) (American Health Packaging) (2020-03-24T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (60687-0468) (American Health Packaging)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (53746-0137) (Amneal Pharmaceuticals LLC) (2010-01-21T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (53746-0466) (Amneal Pharmaceuticals LLC) (2019-07-16T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (65162-1103) (Amneal Pharmaceuticals LLC) (2015-03-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (69238-1103) (Amneal Pharmaceuticals LLC) (2019-03-11T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (65162-0466) (Amneal Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (67877-0121) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2012-02-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (67877-0121) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2015-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (67877-0296) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (67877-0321) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (67877-0321) (Ascend Laboratories, LLC a Subsidiary of Alkem Laboratories Ltd) (2016-05-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (59651-0362) (Aurobindo Pharma Limited)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (42291-0339) (AvKARE, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (42291-0428) (AvKARE, Inc.) (2023-09-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (42291-0442) (AvKARE, Inc.) (2024-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (42582-0113) (Bi-Coastal Pharmaceutical Corp.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (69150-0800) (Biomes Pharmaceuticals, LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (10544-0071) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (10544-0024) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (10544-0431) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (10544-0613) (Blenheim Pharmacal, Inc.) (2017-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (51991-0740) (Breckenridge Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (62135-0402) (Chartwell RX LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (55111-0103) (Dr. Reddy's Laboratories, Inc.) (2008-01-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (55111-0684) (Dr. Reddy's Laboratories, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (51293-0845) (ECI Pharmaceuticals )
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (49884-0216) (Endo USA, Inc.) (2005-04-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (76282-0714) (Exelan Pharmaceuticals, Inc.)

Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (71921-0182) (Florida Pharmaceutical Products, LLC.)

Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (60429-0221) (Golden State Medical Supply, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (51407-0371) (Golden State Medical Supply, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (51407-0841) (Golden State Medical Supply, Inc.)

Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (52959-0077) (HJ Harkins Co Inc)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (52959-0077) (HJ Harkins Co Inc)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (61808-0130) (Imiren Pharmaceuticals Inc) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (50742-0159) (Ingenus Pharmaceuticals, LLC) (2015-11-02T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (53746-0137) (Interpharm Inc) (2008-06-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (68645-0222) (Legacy Pharmaceutical Packaging, LLC) (2017-04-30T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (68645-0476) (Legacy Pharmaceutical Packaging, LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (68645-0531) (Legacy Pharmaceutical Packaging, LLC) (2019-05-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (68645-0563) (Legacy Pharmaceutical Packaging, LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00904-5187) (Major Pharmaceuticals Inc, a Harvard Drug Group Company) (2013-07-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00904-5855) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00904-5855) (Major Pharmaceuticals Inc, a Harvard Drug Group Company)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (63739-0691) (McKesson Packaging) (2020-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (63739-0137) (McKesson Packaging Inc) (2011-02-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (63739-0444) (McKesson Packaging Inc) (2015-08-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (58657-0682) (Method Pharmaceuticals)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (55370-0535) (Mova Pharmaceuticals Corp) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (51079-0596) (Mylan Institutional LLC) (2010-10-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (59762-7380) (Mylan Pharmaceutiacals, Inc.) (2006-09-05T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00378-0801) (Mylan Pharmaceuticals Inc.) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00378-1801) (Mylan Pharmaceuticals Inc.) (2005-04-08T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (66267-0118) (NuCare Pharmaceuticals Inc) (2008-04-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (66267-0963) (NuCare Pharmaceuticals Inc) (2008-04-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00603-4020) (Par Health USA, LLC) (2009-12-04T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00603-4023) (Par Health USA, LLC) (2011-02-09T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (55289-0140) (PD-Rx Pharmaceuticals, Inc.) (2015-04-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (43063-0013) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (55289-0140) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (43063-0847) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (43063-0858) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (43063-0914) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (43063-0858) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (55289-0140) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (72789-0186) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (72789-0200) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (72789-0218) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (72789-0364) (PD-Rx Pharmaceuticals, Inc.)
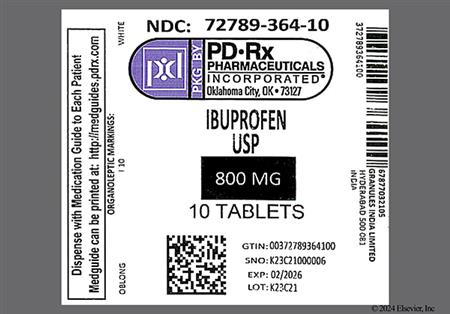
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (72789-0382) (PD-Rx Pharmaceuticals, Inc.)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (52605-0123) (Polygen Pharmaceuticals LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (49999-0042) (Quality Care Products, LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (17236-0570) (R&S Northeast, LLC, formerly Dixon-Shane Drug Company) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (33358-0188) (RxChange Co.) (2024-12-31T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00781-1363) (Sandoz, Inc. a Novartis Company) (2005-04-25T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00364-2137) (Schein Pharmaceutical Inc, an Actavis Company) (2005-09-06T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (73086-0212) (Skya Health, LLC)

Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (70436-0182) (Slate Run Pharmaceuticals, LLC)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (70512-0780) (Sola Pharmaceuticals)

Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (60760-0135) (St. Mary's Medical Park Pharmacy)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (42543-0964) (Strides Pharma Inc)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (64380-0807) (Strides Pharma Science Limited)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00677-1119) (Sun Pharmaceutical Industries, Inc.) (2008-03-06T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00182-1297) (Teva Pharmaceuticals USA) (2009-08-13T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (50111-0451) (Teva Pharmaceuticals USA) (2005-01-28T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00172-3648) (Teva Pharmaceuticals USA) (2008-03-20T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00591-2137) (Teva/Actavis US) (2005-08-24T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00591-3466) (Teva/Actavis US) (2008-08-29T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (00591-3665) (Teva/Actavis US) (2010-02-11T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (49483-0604) (Time Cap Laboratories Inc)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (71550-0100) (Virtue Rx, LLC) (2018-03-01T00:00:00)
Ibuprofen Oral tablet
Ibuprofen 800mg Tablet (69367-0396) (Westminster Pharmaceuticals, LLC)

Ibuprofen Oral tablet
Motrin 800mg Tablet (00009-7387) (Pfizer Inc.) (2007-11-01T00:00:00)
Ibuprofen Oral tablet
Samson-8 800mg Tablet (61406-0374) (Ultras Pharmaceuticals Inc) (2024-12-31T00:00:00)
Ibuprofen Solution for injection
Caldolor 800mg/200mL Solution for Injection (66220-0284) (Cumberland Pharmaceuticals)
Ibuprofen Solution for injection
Caldolor 400mg/4ml Solution for Injection (66220-0247) (Cumberland Pharmaceuticals) (2011-01-01T00:00:00)
Ibuprofen Solution for injection
Caldolor 800mg/8mL Solution for Injection (66220-0287) (Cumberland Pharmaceuticals)
Description / Classification
Description
Ibuprofen is an oral and intravenous non-steroidal anti-inflammatory drug (NSAID) indicated for the treatment of mild to severe pain, osteoarthritis, rheumatoid arthritis, juvenile rheumatoid arthritis/juvenile idiopathic arthritis, dysmenorrhea, and fever. All NSAIDs, including ibuprofen, cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and GI perforation of the esophagus, stomach, small intestine, or large intestine and are associated with an increased risk of serious cardiovascular (CV) thromboembolism, including myocardial infarction or stroke. Use the lowest effective dose for the shortest possible duration; the increase in CV risk has been most consistently observed at higher doses.[30569][35893][44121][55095]
Classification
Diagnostic Agents
Diagnostic Agents, Other
Musculo-Skeletal System
Antiinflammatory Agents and Antirheumatic Agents
Antiinflammatory and Antirheumatic Agents
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Administration Information
General Administration Information
For storage information, see the specific product information within the How Supplied section.
Route-Specific Administration
Injectable Administration
Visually inspect parenteral products for particulate matter and discoloration prior to administration whenever solution and container permit. If visibly opaque particles, discolorations, or other foreign material are observed, do not use the solution.
The patient must be well hydrated prior to administration to reduce the risk of renal adverse events.
Avoid administration of more than 1 NSAID at a time.[35893]
Intravenous Administration
Dilution
Dilute to a final concentration of 4 mg/mL or less in compatible diluent (0.9% Sodium Chloride Injection, Lactated Ringer's Injection, or Dextrose 5% Injection) prior to administration.
100 mg dose: Dilute 1 mL ibuprofen in at least 100 mL diluent.
200 mg dose: Dilute 2 mL ibuprofen in at least 100 mL diluent.
400 mg dose: Dilute 4 mL ibuprofen in at least 100 mL diluent.
800 mg dose: Dilute 8 mL ibuprofen in at least 200 mL diluent.
For pediatric weight-based dosing: ensure final concentration is 4 mg/mL or less.
Intravenous infusion
Infuse over at least 30 minutes for adults and over at least 10 minutes for pediatric patients.
Storage: Diluted solutions are stable for 24 hours at ambient temperature (approximately 20 to 25 degrees C) and room lighting.[35893]
Adverse Reactions
Severe
agranulocytosis
anaphylactoid reactions
aplastic anemia
arrhythmia exacerbation
aseptic meningitis
azotemia
bradycardia
erythema multiforme
GI bleeding
GI perforation
hearing loss
heart failure
hemolytic anemia
lupus-like symptoms
optic neuritis
pancreatitis
peptic ulcer
renal failure (unspecified)
renal papillary necrosis
serum sickness
Stevens-Johnson syndrome
toxic epidermal necrolysis
visual impairment
angioedema
apnea
bronchospasm
coma
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
esophageal stricture
esophageal ulceration
exfoliative dermatitis
glomerulonephritis
hematemesis
hepatic failure
hepatic necrosis
hyperkalemia
interstitial nephritis
myocardial infarction
nephrotic syndrome
odynophagia
oliguria
pancytopenia
proteinuria
renal tubular necrosis
seizures
stroke
thromboembolism
vasculitis
Moderate
anemia
constipation
edema
fluid retention
hypokalemia
neutropenia
prolonged bleeding time
thrombocytosis
elevated hepatic enzymes
hypernatremia
peripheral edema
urinary retention
amblyopia
blurred vision
bullous rash
cataracts
confusion
conjunctivitis
cystitis
depression
eosinophilia
hallucinations
hematuria
hepatitis
hypertension
hypoglycemia
jaundice
melena
metabolic acidosis
palpitations
pseudotumor cerebri
scotomata
sinus tachycardia
thrombocytopenia
chest pain (unspecified)
diagnostic test interference
dysphagia
dyspnea
dysuria
esophagitis
fixed drug eruption
gastritis
glossitis
hyperglycemia
hyperuricemia
hyponatremia
hypotension
infertility
leukopenia
lymphadenopathy
medication overuse headache
photophobia
respiratory depression
stomatitis
wheezing
withdrawal
Mild
abdominal pain
diarrhea
dizziness
dyspepsia
flatulence
headache
maculopapular rash
nausea
pruritus
pyrosis (heartburn)
rash
tinnitus
vomiting
anorexia
cough
injection site reaction
alopecia
diplopia
drowsiness
emotional lability
epistaxis
gynecomastia
insomnia
menorrhagia
paresthesias
photosensitivity
polyuria
urticaria
vesicular rash
xerophthalmia
xerostomia
anxiety
asthenia
diaphoresis
ecchymosis
eructation
fever
infection
malaise
purpura
rhinitis
syncope
tremor
vertigo
weight gain
weight loss
The most frequent type of adverse reaction reported with orally administered ibuprofen is gastrointestinal (GI). In controlled trials, the overall incidence of GI adverse reactions associated with oral ibuprofen was about half that seen in aspirin- or indomethacin-treated patients. Severe GI effects occur in patients taking ibuprofen with a frequency of less than 1% and include peptic ulcer (gastric or duodenal ulcer with GI bleeding and/or GI perforation), gastrointestinal hemorrhage, and melena. Inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine can be fatal and may occur at any time, with or without warning symptoms. Only 20% of patients who develop a serious upper GI event is symptomatic. The risk of severe GI events is increased by the presence of the following factors: history of peptic ulcer disease or GI bleed, smoking, alcohol usage, concomitant usage of anticoagulants, or oral corticosteroids, older age, poor general health status, and NSAID duration of use. Upper GI ulcers, gross bleeding, or perforation occur in approximately 1% of patients treated for 3 to 6 months, and in about 2 to 4% of patients treated for one year. Gastrointestinal bleeding or erosive gastritis can be minor or life-threatening and may result from a combination of direct irritant action on the stomach mucosa and an increased bleeding time, due to changes in platelet aggregation. Older patients appear to be greater affected by GI ulceration or bleeding; most fatal GI events occur in older or debilitated patients. Occult GI bleeding occurs in many patients and is not necessarily correlated with GI distress. Although the amount of blood lost is usually not significant, patients may become anemic as a result of iron deficiency. Patients on prolonged therapy should undergo regular blood monitoring. Nausea, vomiting, dyspepsia, and flatulence have been reported in 1 to 10% of patients receiving oral ibuprofen and in patients treated with intravenous ibuprofen for post-operative pain at similar rates to those receiving placebo. In pediatric intravenous ibuprofen trials, nausea and vomiting were among the most common adverse events, occurring at an incidence > 2%.[35893] Other adverse GI effects reported in 1 to 10% of patients receiving oral ibuprofen include abdominal pain, bloating, constipation, diarrhea, epigastric pain, and pyrosis (heartburn). Abdominal distress, indigestion, decreased appetite, and abdominal cramps were reported in > 1% and < 3% of ibuprofen-treated patients. Xerostomia and gingival ulcer were reported with ibuprofen in < 1% of patients. Duodenitis, glossitis, hematemesis, eructation, hepatorenal syndrome, appetite changes, and rectal bleeding may also occur. Use the lowest effective dose of ibuprofen for the shortest possible duration. Discontinue ibuprofen if a serious GI adverse event is suspected.[44120] [44121]
Rare cases of esophagitis have been reported in patients receiving ibuprofen tablets.[44121] Ibuprofen-induced esophagitis is characterized by sudden onset odynophagia, pyrosis (heartburn), retrosternal pain, and dysphagia. Severe complications such as esophageal ulceration, esophageal stricture, bleeding, and perforation have been reported rarely. Risk factors for ibuprofen-induced esophageal effects include taking the medication without water and at night. Symptoms usually resolve within days to weeks after stopping the medication.
Pancreatitis has been reported in < 1% of patients receiving oral ibuprofen.[44120] [44121]
Amblyopia, xerophthalmia, and altered vision (blurred vision, visual impairment, scotomata, and changes in color vision) have been reported with a probable causal relationship in < 1% of patients receiving oral ibuprofen. If a patient develops visual changes, ibuprofen should be discontinued and an ophthalmologic examination with central visual fields and color vision testing should be performed. Vision generally improves when the drug is discontinued. The mechanism for visual disturbances is unclear. Conjunctivitis, diplopia, optic neuritis and cataracts have been reported in < 1% of patients taking ibuprofen; however, a causal relationship is unknown. Tinnitus has been reported in 1—10% and hearing loss in < 1% of ibuprofen-treated patients.[44120] [44121] A prospective analysis examining the association between analgesic use and the risk of hearing loss was conducted in 62,261 women 31—48 years of age at study enrollment who were originally enrolled in the Nurses' Health Study II. Self-reported hearing loss and analgesic use (including acetaminophen, aspirin, and NSAIDs) were examined over 14 years. During 764,247 person-years of follow-up, 10,012 cases of hearing loss were reported. After adjustment for confounders, ibuprofen use >= 2 days per week was independently associated with an increased risk of hearing loss, with the relative risk of hearing loss increasing with increasing frequency of use. Ibuprofen use 2—3, 4—5, or >= 6 days per week was associated with relative risks of 1.13 (95% CI 1.06—1.19), 1.21 (95% CI 1.11—1.32), and 1.24 (95% CI 1.14—1.35), respectively, with a p trend of < 0.0001. Of note, those with more frequent use of ibuprofen were older, had higher body mass indices, were more likely to be past or current smokers, have hypertension, or have diabetes.[53720] In a similar study of male patients, the association between professionally diagnosed hearing loss and analgesic use (including acetaminophen, aspirin, and NSAIDs) was prospectively analyzed in 26,917 patients 40—74 years at study enrollment over 18 years. During 369,079 person-years of follow-up, 3488 cases of hearing loss were reported. After adjustment for confounders, the hazard ratio (HR) for NSAID (e.g., ibuprofen) associated hearing loss was 1.21 (95% CI 1.11—1.33, p = 0.1) in patients who were regular users of the drug (>= 2 times weekly) compared to those with less use. Men who regularly used NSAIDs for >= 4 years were 33% (18—49%) more likely to develop hearing loss than those with shorter use. Regular users < 50 years of age were 61% more likely to develop hearing loss compared to non-regular users; regular users 50—59 years had a 32% higher risk of hearing loss, and regular users >= 60 years had a 16% higher risk.[53719] These studies do suggest association; however, data are based on patient reporting of the outcomes. Information regarding noise exposure and analgesic doses was not provided.[53719] [53720] Ibuprofen or NSAID related ototoxicity may result from several mechanisms, including reduced cochlear blood flow, impairment of outer hair cell function, or inhibition of prostaglandin forming cyclooxygenase.[53720] As a true long-term association may exist, counsel patients to minimize long-term treatment with ibuprofen as much as possible.
Ibuprofen has been associated with acute renal failure (unspecified) in patients with pre-existing significantly impaired renal function, decreased creatinine clearance, polyuria, azotemia, cystitis, and hematuria in less than 1% of patients. Abnormal renal function is among the most frequently reported adverse events with ibuprofen or other NSAIDs, occurring in approximately 1% to 10% of patients. It is well known that vasodilatory renal prostaglandins and the potent vasoconstrictor angiotensin II work in concert to maintain renal blood flow. Inhibition of renal prostaglandins by NSAIDs can cause renal insufficiency. This problem can manifest as hyperkalemia, hyperuricemia, or azotemia. Hyperkalemia and other increases in serum potassium concentrations have been reported in patients without renal impairment taking NSAIDs, likely due to a hyporeninemic-hypoaldosteronism state.[35893] Renal papillary necrosis has been reported in less than 1% of ibuprofen-treated patients, and has been associated with long-term administration of NSAIDs. With some NSAIDS, nephrotic syndrome, proteinuria, and interstitial nephritis have been reported. Dysuria, oliguria, glomerulonephritis, and renal tubular necrosis have also been reported with the use of ibuprofen. Inhibition of prostaglandin synthesis by NSAIDs potentiates water reabsorption. Fluid retention and edema (peripheral edema) have been reported in 1% to 10% of patients receiving ibuprofen.[44120] [44121] Urinary retention (3% to 5%) and increased blood urea (10%) have been reported during adult IV ibuprofen clinical trials.[35893] Hyponatremia due to water intoxication has been reported with NSAID use.[33608] [33609] [33610] Monitoring of the patient's fluid status and serum creatinine and blood urea nitrogen concentrations is recommended.
Like all NSAIDs, ibuprofen-induced increases in water retention and decreases in renal perfusion may exacerbate pre-existing cardiovascular complications, including hypertension (less than 1%) and congestive heart failure (specifically in patients with marginal cardiac function, less than 1%).[44120] [44121] Further, NSAIDs may increase the risk of serious cardiovascular thromboembolism, myocardial infarction, and stroke, which can be fatal. Estimates of increased relative risk range from 10% to 50% or more, based on the drug and dose studied. The risk may increase with increased exposure, as measured in dose or duration. Significant cardiovascular risk has been observed within days to weeks of NSAID initiation. The relative increase in cardiovascular thrombotic events over baseline appears to be similar in patients with or without cardiovascular disease or risk factors for cardiovascular disease; however, patients with known cardiovascular disease or risk factors may be at greater risk because of a higher baseline risk of events.[59937] While comprehensive data regarding relative cardiovascular safety of any particular NSAID compared to other NSAIDs is not available, celecoxib 100 mg twice daily was shown to be non-inferior to ibuprofen 600 to 800 mg 3 times daily or naproxen 375 to 500 mg twice daily for the composite endpoint of cardiovascular death, nonfatal MI, and nonfatal stroke in osteoarthritis or rheumatoid arthritis adult patients with or at high risk for cardiovascular disease. The intention-to-treat (ITT) analysis followed patients for 30 months, with 8,072 patients randomized to celecoxib, 8,040 randomized to ibuprofen, and 7,969 randomized to naproxen. ITT hazard ratios (95% CI) were 0.93 (0.76 to 1.13) for celecoxib vs. naproxen, 0.86 (0.7 to 1.04) for celecoxib vs. ibuprofen, and 1.08 (0.89 to 1.31) for ibuprofen vs. naproxen. Average 24-hour systolic pressure decreased by 0.3 mmHg in patients receiving celecoxib in a 4-month substudy of 444 patients, while average 24-hour systolic pressures increased by 3.7 mmHg and 1.6 mmHg in patients taking ibuprofen and naproxen, respectively.[56268] There is no consistent evidence that concomitant use of aspirin mitigates the increased risk for cardiovascular thrombotic events. In observational studies, data demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality; the incidence of death in the first year post-MI in NSAID-treated patients was 20 per 100 person years compared to 12 per 100 person years in non-NSAID exposed patients. An increased relative risk of death in NSAID users was observed across 4 years of follow-up. A meta-analysis of randomized, controlled trials demonstrated an approximate 2-fold increase in hospitalizations for heart failure among nonselective- and COX-2 selective NSAID-treated patients compared to placebo.[35893] Other cardiovascular events reported in ibuprofen-treated patients include: palpitations (less than 1%; probable causal relationship), arrhythmia exacerbation (less than 1%), sinus tachycardia (less than 1%), sinus bradycardia (less than 1%), syncope, hypotension, and vasculitis. Some patients have experienced chest pain (unspecified) during postmarketing use of ibuprofen. Inform patients of the signs and symptoms of CV events, and advise them to seek medical help immediately if such signs or symptoms occur.[44120] [44121] [44130]
Borderline elevated hepatic enzymes have been reported in up to 15% of patients receiving NSAID therapy; elevated hepatic enzymes have been reported in <= 10% of ibuprofen-treated patients. These abnormalities may persist, progress, or be transient. One percent of patients in clinical trials with NSAIDs had elevations of ALT or AST greater than or equal to 3 times normal values. Rarely, NSAIDs have been associated with hepatotoxicity including jaundice (< 1%), hepatitis (< 1%), hepatic necrosis, and hepatic failure. Ongoing monitoring is recommended in patients who develop signs or symptoms of liver dysfunction and/or with abnormal LFTs. Discontinue ibuprofen in patients with evidence of new onset liver disease.[44120][44121]
Prolonged bleeding time is among the most frequently reported adverse events that occur with ibuprofen or other NSAIDs (1% to 10%). The incidence of neutropenia is less than 1% for oral therapy and 7% to 13% for parenteral therapy. Anemia has been reported in 1% to 10% of subjects treated with oral ibuprofen or other NSAIDs, and in 17% to 20% of adults and more than 2% of pediatric individuals treated with parenteral ibuprofen. This may be related to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis. NSAIDs may increase the risk of bleeding events. If an individual treated with an NSAID has any signs or symptoms of anemia, monitor hemoglobin or hematocrit. Consider monitoring a complete blood count (CBC) periodically in individuals on long-term NSAID treatment. Other hematologic effects (less than 1%) due to oral ibuprofen include agranulocytosis, aplastic anemia, hemolytic anemia (sometimes Coombs positive), thrombocytopenia with or without purpura, eosinophilia, decreases in hemoglobin and hematocrit, and bleeding episodes including epistaxis and menorrhagia. Ecchymosis, leukopenia, purpura, stomatitis, lymphadenopathy, and pancytopenia have been reported with oral ibuprofen. Subjects receiving parenteral ibuprofen also experienced hypoalbuminemia (3% to 10% ibuprofen vs. 4% placebo) and thrombocythemia/thrombocytosis (3% to 10%).[35893] [44120] [44121]
NSAIDs can cause serious and potentially fatal skin reactions, including exfoliative dermatitis, Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and fixed drug eruption (FDE), which may present as a more severe variant known as generalized bullous fixed drug eruption (GBFDE). These serious events may occur without warning. Inform individuals about the signs and symptoms of serious skin reactions and instruct them to discontinue use of the NSAID at the first appearance of skin rash or any other sign of hypersensitivity. Pruritus and rash, including maculopapular rash, were reported with ibuprofen or other NSAIDs in 1% to 10% of subjects in clinical trials. Other dermatologic reactions reported with ibuprofen in less than 1% of subjects include alopecia, bullous rash, erythema multiforme, photosensitivity, SJS, TEN, urticaria, and vesicular rash. Diaphoresis has been occasionally reported with ibuprofen or other NSAIDs. Exfoliative dermatitis, FDE, SJS, and TEN have been reported with ibuprofen during postmarketing experience.[44120] [44121]
Ibuprofen may cause bronchospasm, dyspnea, and wheezing in patients with asthma. The proposed mechanism of nonsteroidal antiinflammatory drug-sensitive asthma is excessive production of cysteinyl leukotrienes. A single exposure could induce lung function deterioration, as the reaction is not thought to be of an allergic hypersensitivity nature. Likewise, subsequent exposures should not result in escalating bronchospasm severity. Other respiratory-related adverse reactions that have been reported rarely include: apnea, respiratory depression, pneumonia, and rhinitis.[44120] [44121] Cough (3% or less) and bacterial pneumonia (3% to 10%) were reported with parenteral ibuprofen-treated patients during adult trials for postoperative pain and fever, respectively.[35893]
Dizziness, headache, and nervousness have been reported in 1% to 10% of patients taking ibuprofen or other NSAIDs; patients receiving parenteral ibuprofen in clinical trials experienced dizziness and headache.[35893] [44120] [44121] In pediatric intravenous ibuprofen trials, headache was among the most common adverse events, occurring at an incidence more than 2%.[35893] Overuse of drugs for treating acute headaches, including ibuprofen, may lead to medication overuse headache. Patients may experience migraine-like daily headaches or a significant increase in migraine attack frequency. Discontinuation of the overused drug and treatment of withdrawal symptoms (e.g., transient worsening of headache) may be necessary. Advise patients about the risks of medication overuse (e.g., use of ibuprofen for at least 15 days/month or any combination of therapy for 10 days/month) and encourage them to keep a written record of headache frequency and drug use.[66767] [66803] Pediatric guidelines recommend no more than 14 days/month of over-the-counter medication and no more than 9 days/month of any combination of therapy to avoid medication overuse headache.[64587]
Aseptic meningitis has been reported in < 1% of patients taking ibuprofen.[44120] [44121] Ibuprofen has been the most common NSAID implicated in this adverse reaction; however, cases have been reported with sulindac, naproxen, tolmetin, diclofenac, ketoprofen, rofecoxib, and piroxicam. No cases of aseptic meningitis were reported among patients receiving intravenous ibuprofen in clinical trials. Aseptic meningitis from one NSAID does not preclude use of another NSAID; most patients can be treated with another drug without incident. However, one patient with Sjogren's syndrome experienced aseptic meningitis after receipt of naproxen, ibuprofen, and rofecoxib at different times; aseptic meningitis developed about a week after each drug exposure, and the symptoms abated roughly 2 days following each drug cessation.[27710] The occurrence of aseptic meningitis is not related to NSAID chemical class or prostaglandin inhibition. A Type III or IV immunological hypersensitivity reaction is the proposed mechanism of action. Drug-induced aseptic meningitis usually occurs shortly after drug initiation but can occur after years of drug usage. Although NSAID-induced aseptic meningitis is primarily reported in patients with systemic lupus erythematosus (SLE), healthy patients and patients with other disease states such as ankylosing spondylitis, connective tissue disease, osteoarthritis, and rheumatoid arthritis have developed NSAID-induced aseptic meningitis. Symptoms of aseptic meningitis include feeling confused, somnolence, general feeling of illness, severe headache, nausea, nuchal rigidity, and photophobia. As aseptic meningitis is a diagnosis of exclusion, the suspected drug should be discontinued and not restarted unless a rechallenge is desired.
Oral ibuprofen has been associated infrequently (< 1%; without causal relationship) with the development of pseudotumor cerebri (benign intracranial hypertension).[44120]
CNS-related adverse reactions with a probable causal relationship reported in < 1% of ibuprofen-treated patients include: depression, insomnia, confusion, emotional lability, and drowsiness. Those reactions reported in < 1% of patients where the causal relationship to ibuprofen has not been established include: paresthesias, hallucinations, and dream abnormalities. Other CNS-related adverse reactions that have been reported occasionally or rarely include anxiety, asthenia, malaise, tremor, vertigo, seizures and coma.[44120][44121]
Fever, infection, and sepsis have been reported in patients receiving ibuprofen.[44121]
Allergic reactions with a probable causal relationship to ibuprofen that include a syndrome of abdominal pain, fever, chills, nausea, vomiting, anaphylaxis (anaphylactoid reactions), and bronchospasm have been reported in less than 1% of patients. Other allergic reactions without an established causal relationship to ibuprofen reported in less than 1% of patients include serum sickness, lupus erythematosus syndrome (lupus-like symptoms), Henoch-Schonlein vasculitis, and angioedema.[44120] [44121]
Decreased appetite (anorexia) has been reported in 1% to 3% of patients taking ibuprofen during clinical trials. Gynecomastia, hypoglycemia, and metabolic acidosis have been reported with ibuprofen in less than 1% of patients, although a causal relationship has not been established. Weight changes (weight gain, weight loss) and hyperglycemia have also been reported.[44120] [44121] Metabolic abnormalities including hypokalemia (19% or less), hypoproteinemia (10% to 13%), and hypernatremia (7% to 10%) were reported during adult clinical trials for parenteral ibuprofen.[35893]
In pediatric intravenous ibuprofen trials, infusion site pain (injection site reaction) was among the most common adverse events, occurring at an incidence > 2%.[35893]
NSAIDs, such as ibuprofen, may delay or prevent prostaglandin-mediated rupture of ovarian follicles, which has been associated with reversible infertility. Small studies of women treated with NSAIDs demonstrated a reversible delay in ovulation. Consider withdrawal of NSAIDs in women who have difficulties conceiving or who are undergoing infertility evaluation.[35893]
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), a multi-organ hypersensitivity reaction, has occurred with NSAIDs. Some of these events have been life-threatening or fatal. DRESS typically presents as fever, rash, and/or lymphadenopathy in conjunction with other organ system involvement including hepatitis, nephritis, hematologic abnormalities, myocarditis, or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. Early manifestations such as fever and lymphadenopathy may be present without evidence of a rash. Discontinue the NSAID in patients presenting with such signs and symptoms in whom an alternative etiology cannot be identified.[35893]
The pharmacological activity of NSAIDS in reducing inflammation, and possibly fever, may result in diagnostic test interference by diminishing the utility of these diagnostic signs in detecting infection.[44120]
Contraindications / Precautions
aspirin exacerbated respiratory disease
coronary artery bypass graft surgery (CABG)
asthma
bleeding disorder
breast-feeding
cardiovascular disease
collagen-vascular disease
ethanol ingestion
geriatric
GI bleeding
hepatic disease
hypovolemia
people who may become pregnant
peptic ulcer disease
pregnancy
renal disease
reproductive risk
serious cardiovascular events
serious gastrointestinal events
tobacco smoking
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Ibuprofen is contraindicated in the setting of coronary artery bypass graft surgery (CABG). An increased incidence of myocardial infarction and stroke was found in clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days after CABG surgery. NSAIDs may increase the risk of serious cardiovascular events, which can be fatal.[35893] [44120] Guidelines recommend against NSAID use in individuals presenting with and hospitalized for ST-elevation myocardial infarction (STEMI) due to increased risk of mortality and cardiovascular (CV) complications associated with their use.[55688] Avoid NSAID use in individuals with a recent myocardial infarction unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If an NSAID is used in individuals with a recent myocardial infarction, monitor for signs of cardiac ischemia. Observational data from a national registry demonstrated that individuals treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning the first week of treatment. An increased relative risk of death in NSAID users continued during the follow-up period of 4 years. Data demonstrate that individuals treated with NSAIDs were more likely to die in the first year after a myocardial infarction compared to those not treated with NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease; however, individuals with known cardiovascular disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment with an NSAID; the increase in CV thrombotic risk has been observed most consistently at higher doses. Current evidence is insufficient to determine if the risk of an event is higher or lower for any particular NSAID compared to other NSAIDs. There is no consistent evidence that concomitant use of aspirin mitigates the increased risk for CV thrombotic events. To minimize the potential risk for an adverse CV event in NSAID-treated individuals, use the lowest effective dose for the shortest duration possible; remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. NSAIDs may worsen pre-existing hypertension, which may contribute to the increased incidence of CV events. Monitor blood pressure during NSAID treatment initiation and throughout therapy. Avoid NSAID use in individuals with severe heart failure, unless the benefits of treatment are expected to outweigh the risks. Monitor for signs of worsening heart failure if an NSAID is used in individuals with severe heart failure. Monitor renal function in individuals with heart failure during use of an NSAID. Data demonstrate an increased risk for myocardial infarction, hospitalization for heart failure, and death with NSAID use in individuals with heart failure.[35893] [44120]
Ibuprofen is contraindicated in individuals with aspirin exacerbated respiratory disease, which may include chronic rhinosinusitis complicated by nasal polyps, severe and potentially fatal acute bronchospasm, and/or intolerance to aspirin and other NSAIDs. When an NSAID is used in individuals with pre-existing asthma without known aspirin sensitivity, monitor for changes in the signs and symptoms of asthma.[35893] [44120]
Individuals with a prior history of GI bleeding and/or peptic ulcer disease who use NSAIDs had a more than 10-fold increased risk of developing a GI bleed compared to individuals without these risk factors. Individuals with advanced hepatic disease or bleeding disorder are also at increased risk for GI bleeding. Other risk factors for GI bleeding in individuals receiving NSAIDs include longer duration of NSAID therapy, concomitant use of oral corticosteroids, aspirin, anticoagulants, or SSRIs, tobacco smoking, ethanol ingestion, older age, and poor general health status. Coadministration with certain medications, specifically aspirin or other NSAIDs, is contraindicated due to the cumulative risk of inducing serious NSAID-related adverse events; concomitant use of ketorolac with aspirin or other NSAIDs increases the risk of GI toxicity, with little or no increase in efficacy. Serious gastrointestinal events, including bleeding, inflammation, perforation, and ulceration, can occur at any time and without warning symptoms in individuals receiving NSAIDs. To minimize the risk of an adverse GI event in NSAID-treated individuals, use the lowest effective NSAID dose for the shortest possible duration. Avoid concurrent administration of other NSAIDs; in the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor more closely for evidence of GI bleeding. Avoid NSAID use in individuals at higher risk for GI adverse events unless benefits are expected to outweigh the increased bleeding risk, and consider alternate therapies other than NSAIDs for those individuals and individuals with active GI bleeding. Monitor individuals for signs and symptoms of GI bleeding and ulceration during NSAID therapy.[35893] [44120]
Monitor renal function in individuals with hepatic impairment during use of an NSAID. NSAID use in individuals with hepatic failure in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion may precipitate renal decompensation. Advanced hepatic disease is also a risk factor for GI bleeding in individuals who use NSAIDs.[35893] [44120]
Avoid NSAID use in individuals with advanced renal disease, unless the benefits are expected to outweigh the risks of worsening renal function. If an NSAID is used in individuals with advanced renal disease, monitor for signs and symptoms of worsening renal function. Correct volume status in individuals with dehydration or hypovolemia prior to starting an NSAID. Monitor renal function in individuals with renal impairment, dehydration, or hypovolemia during use of an NSAID. NSAID use in individuals with renal impairment, dehydration, or hypovolemia in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion may precipitate renal decompensation. The renal effects of NSAIDs may hasten the progression of renal dysfunction in individuals with pre-existing renal disease.[35893] [44120]
Aseptic meningitis has been reported with ibuprofen and is probably more likely to occur in individuals with systemic lupus erythematosus and related collagen-vascular disease.[35893] [44120]
Geriatric adults, compared to younger individuals, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the older adult outweighs these potential risks, start NSAID dosing at the low end of the dosing range, and monitor for adverse effects.[32122] According to the Beers Criteria, NSAIDs are considered potentially inappropriate medications (PIMs) in geriatric adults. There is an increased risk of GI bleeding and peptic ulcer disease in high-risk groups including those older than 75 years, or those taking systemic corticosteroids, anticoagulants, or antiplatelet medications. The risk of GI ulcers, gross bleeding, or perforation is cumulative with continued use. Avoid the chronic use of NSAIDs in high-risk individuals, including those with a history of gastric or duodenal ulcers, unless other alternatives are not effective, and the individual can take a gastroprotective agent. The use of a gastroprotective agent, like a proton pump inhibitor or misoprostol, reduces but does not eliminate GI risks. NSAIDs may also increase blood pressure and induce kidney injury. Avoid use of NSAIDs in geriatric adults with the following conditions due to the potential for symptom exacerbation or adverse effects: symptomatic heart failure (fluid retention, symptom exacerbation) or chronic kidney disease Stage 4 or higher (CrCl less than 30 mL/minute) (acute kidney injury, further decline of renal function). Use with caution in individuals with asymptomatic heart failure.[63923]
Avoid the use of NSAIDs, such as ibuprofen, during pregnancy starting at 30 weeks gestation due to the risk of premature closure of the fetal ductus arteriosus. When use is necessary between 20 and 30 weeks gestation, limit use to the lowest effective dose and shortest duration possible. Consider ultrasound monitoring of amniotic fluid if treatment exceeds 48 hours. Discontinue the NSAID if oligohydramnios develops, and follow up according to clinical practice. Use of NSAIDs around 20 weeks gestation and later may also cause fetal renal dysfunction, leading to oligohydramnios, and in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. Oligohydramnios is often, but not always, reversible with treatment discontinuation. Complications of prolonged oligohydramnios may include limb contractures and delayed lung maturation. In some cases, invasive neonatal procedures such as exchange transfusion or dialysis have been required. Observational data regarding other potential embryo-fetal risks of NSAID use during the first or second trimesters are inconclusive. Animal studies indicate that prostaglandins play an important role in endometrial blood flow, embryo implantation, and fetal kidney development. Inhibiting prostaglandin synthesis has been associated with increased pre- and post-implantation loss and impaired kidney development in animals at NSAID doses relevant to clinical use. The effects of ibuprofen on labor and obstetric delivery are unknown. In animal studies, NSAIDs inhibit prostaglandin synthesis, delay parturition, and increase the incidence of still birth.[30569] [35893] [66040]
Counsel people who may become pregnant about the reproductive risk associated with ibuprofen. NSAIDs may delay or prevent prostaglandin-mediated rupture of ovarian follicles, which has been associated with reversible infertility. Small studies have also shown a reversible delay in ovulation. Consider the withdrawal of NSAIDs in those who have difficulties conceiving or who are undergoing infertility evaluation.[35893]
Ibuprofen is compatible with breast-feeding. Ibuprofen is considered a preferred analgesic or anti-inflammatory agent in lactating individuals. It is present in human milk; however, the amount present is much less than safe doses given to infants.[70364] [70365] Limited published literature reports that orally administered ibuprofen has a relative infant dose (RID) of 0.06% to 0.6% of the breast-feeding individual's weight-adjusted dose.[35893] In a study of milk samples from 13 lactating individuals who took approximately 1,000 mg of ibuprofen daily, the relative infant dose was less than 0.38% of the individual's mean weight-adjusted dose. The relative infant dose was highest when the milk protein content was highest during the colostral phase.[60362]
Mechanism Of Action
Ibuprofen competitively inhibits both COX-1 and COX-2 by blocking arachidonate binding resulting in analgesic, antipyretic, and anti-inflammatory pharmacologic effects. The enzymes COX-1 and COX-2 catalyze the conversion of arachidonic acid to prostaglandin G2 (PGG2), the first step of the synthesis prostaglandins and thromboxanes that are involved in rapid physiological responses. Ibuprofen is effective in cases where inflammation has caused sensitivity of pain receptors (hyperalgesia). It appears prostaglandins, specifically prostaglandins E and F, are responsible for sensitizing the pain receptors; therefore, ibuprofen has an indirect analgesic effect by inhibiting the production of further prostaglandins and does not directly affect hyperalgesia or the pain threshold. Ibuprofen promotes a return to a normal body temperature set point in the hypothalamus by suppressing the synthesis of prostaglandins, specifically PGE2, in circumventricular organs in and near the hypothalamus. Ibuprofen may mask fever in some patients, especially with high or chronic dosing. It appears that the anti-inflammatory effects may be primarily due to inhibition of the COX-2 isoenzyme. However, COX-1 is expressed at some sites of inflammation. COX-1 is expressed in the joints of rheumatoid arthritis or osteoarthritis patients, especially the synovial lining, and it is the primary enzyme of prostaglandin synthesis in human bursitis. Ibuprofen is slightly more selective for COX-1 than COX-2.[54023][55079]
Pharmacokinetics
Ibuprofen is administered orally and intravenously.[35893][44120] The Vd of ibuprofen is dependent on patient age and body temperature; febrile children younger than 11 years have a Vd of approximately 0.2 L/kg while adults have a Vd of approximately 0.12 L/kg.[44121] Ibuprofen is highly protein-bound (more than 99% at 20 mcg/mL); at serum concentrations more than 20 mcg/mL, protein binding is saturated and becomes nonlinear. Ibuprofen is a racemic mixture. The S-isomer is responsible for clinical activity. The R-isomer is thought to be pharmacologically inactive; however, approximately 60% of R-ibuprofen is slowly converted to S-ibuprofen in adults.[35893] The conversion of R-ibuprofen to S-ibuprofen is lower in children compared with adults.[55079] S-ibuprofen is metabolized via hepatic oxidation by CYP2C9 to inactive metabolites. Plasma half-life of ibuprofen is approximately 1.7 to 2.5 hours.[35893][44120][55079] Ibuprofen is eliminated in the urine and excretion is nearly complete within 24 hours after the last dose. After ingestion, 45% to 79% of the dose is excreted as metabolites, while approximately 1% and 14% are excreted as free and conjugated ibuprofen, respectively.[44120] Some biliary excretion may occur.[55079]
Affected cytochrome P450 isoenzymes and drug transporters: CYP2C9
S-ibuprofen is metabolized via hepatic oxidation by CYP2C9 to inactive metabolites. CYP2C9 is polymorphic; CYP2C9(1) is the wild-type, and CYP2C9(2) and CYP2C9(3) are the most common variants. The variant CYP2C9(3) allele decreases enzyme activity to a greater extent than does CYP2C9(2), but clearance of racemic ibuprofen was reduced among all variant genotypes as compared with the wild-type (1/1). Higher S-ibuprofen concentrations led to greater inhibition of COX-1 (reduced thromboxane B2 concentrations) and greater inhibition of COX-2 (reduced prostaglandin E2 concentrations). Importantly, both thromboxane B2 and prostaglandin E2 concentrations were reduced the most among patients with the CYP2C9 genotypes (3/3), (1/3), (2/3), and (2/2).[34462]
•Route-Specific Pharmacokinetics*
Oral Route*
Ibuprofen is rapidly absorbed. Peak concentrations are generally reached 1 to 2 hours after administration.[30569] Ibuprofen absorption is faster when ibuprofen is given under fasting conditions. Administration with food affects the rate, but not the extent of absorption. When given with food, the Tmax is delayed by approximately 30 to 60 minutes, and Cmax is decreased by approximately 30% to 50%.[44121] Time to peak antipyretic effect is 3 to 4 hours and duration of effect is 6 to 8 hours.[63000]
Intravenous Route*
Ibuprofen AUC, Cmax, and half-life means (SD) were 109.3 (28.9) mcg x hour/mL, 39.2 (6.09) mcg/mL, and 2.22 (0.45) hours, respectively, after 400 mg IV over 60 minutes in adults and 192.8 (35.7) mcg x hour/mL, 72.6 (9.61) mcg/mL, and 2.44 (0.31) hours, respectively, after 800 mg IV over 60 minutes in adults. Ibuprofen AUC, Cmax, and half-life means (SD) were 80.7 (29.8) mcg x hour/mL, 61.9 (16.5) mcg/mL, and 1.55 (0.41) hours, respectively, in children 6 to 16 years, 79.2 (29.3) mcg x hour/mL, 64.2 (22.1) mcg/mL, and 1.5 (0.6) hours, respectively, in children 2 to 5 years, 71.1 (26.4) mcg x hour/mL, 59.2 (20.6) mcg/mL, and 1.8 (0.5) hours, respectively, in infants and children 6 months to 1 year, and 69.63 (19.28) mcg x hour/mL, 59.75 (12.85) mcg/mL, and 1.3 hours, respectively, in infants 3 to 5 months after 10 mg/kg IV over 10 minutes. Median Tmax (range) was 10 (10-40) minutes in children 6 to 16 years, 12 (10-46) minutes in children 2 to 5 years, 10 (10-30) minutes in infants and children 6 months to 1 year, and 10 minutes in infants 3 to 5 months after 10 mg/kg IV over 10 minutes.[35893]
•Special Populations*
Hepatic Impairment*
Data have shown that mild hepatic disease does not affect the pharmacokinetics of ibuprofen.[55079] However, in adults with moderate to severe hepatic impairment, the elimination half-life of ibuprofen has been shown to be significantly prolonged.[35603]
Renal Impairment*
Data have shown that mild or moderate renal impairment does not affect the pharmacokinetics of ibuprofen.[55079] Ibuprofen is not recommended in patients with advanced renal disease.[44120]
Pediatrics*
The Vd of ibuprofen (either oral or parenterally administered) is dependent on patient age and body temperature. With single oral doses up to 10 mg/kg, a dose response relationship exists in febrile children.[35893][44121] There is also a correlation between the reduction of fever and drug concentration over time. In children, the antipyretic effect of oral therapy begins within 1 hour and peaks within 3 to 4 hours.[63000] The analgesic effect is similarly acute in nature. The pharmacokinetic parameters of IV ibuprofen were determined in a study of 62 febrile pediatric patients. Median Tmax occurred at the end of infusion and elimination half-life was shorter in pediatric patients compared to adults (1.3 to 1.8 hours vs. 2.2 to 2.4 hours).[35893]
Children and Adolescents 6 to 16 years
Mean (SD) pharmacokinetic parameters of ibuprofen 10 mg/kg IV in 25 febrile patients 6 to 16 years of age were as follows: AUC = 80.7 (29.8) mcg x hour/mL; Cmax = 61.9 (16.5) mcg/mL; half-life = 1.55 (0.41) hours. Median Tmax (range) = 10 (10-40) minutes.[35893]
Children 2 to 5 years
Mean (SD) pharmacokinetic parameters of ibuprofen 10 mg/kg IV in 12 febrile patients 2 to 5 years of age were as follows: AUC = 79.2 (29.3) mcg x hour/mL; Cmax = 64.2 (22.1) mcg/mL; half-life = 1.5 (0.6) hours. Median Tmax (range) = 12 (10-46) minutes.[35893]
Infants and Children 6 months to 1 year
Mean (SD) pharmacokinetic parameters of ibuprofen 10 mg/kg IV in 5 febrile patients 6 months to less than 2 years of age were as follows: AUC = 71.1 (26.4) mcg x hour/mL; Cmax = 59.2 (20.6) mcg/mL; half-life = 1.8 (0.5) hours. Median Tmax (range) = 10 (10-30) minutes.[35893]
Infants 3 to 5 months
Mean (SD) pharmacokinetic parameters of ibuprofen 10 mg/kg IV in 20 febrile patients 3 to 5 months of age were as follows: AUC = 69.63 (19.28) mcg x hour/mL; Cmax = 59.75 (12.85) mcg/mL; half-life = 1.3 hours. Median Tmax = 10 minutes.[35893]
Pregnancy / Breast-Feeding
Pregnancy
Avoid the use of NSAIDs, such as ibuprofen, during pregnancy starting at 30 weeks gestation due to the risk of premature closure of the fetal ductus arteriosus. When use is necessary between 20 and 30 weeks gestation, limit use to the lowest effective dose and shortest duration possible. Consider ultrasound monitoring of amniotic fluid if treatment exceeds 48 hours. Discontinue the NSAID if oligohydramnios develops, and follow up according to clinical practice. Use of NSAIDs around 20 weeks gestation and later may also cause fetal renal dysfunction, leading to oligohydramnios, and in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. Oligohydramnios is often, but not always, reversible with treatment discontinuation. Complications of prolonged oligohydramnios may include limb contractures and delayed lung maturation. In some cases, invasive neonatal procedures such as exchange transfusion or dialysis have been required. Observational data regarding other potential embryo-fetal risks of NSAID use during the first or second trimesters are inconclusive. Animal studies indicate that prostaglandins play an important role in endometrial blood flow, embryo implantation, and fetal kidney development. Inhibiting prostaglandin synthesis has been associated with increased pre- and post-implantation loss and impaired kidney development in animals at NSAID doses relevant to clinical use. The effects of ibuprofen on labor and obstetric delivery are unknown. In animal studies, NSAIDs inhibit prostaglandin synthesis, delay parturition, and increase the incidence of still birth.[30569] [35893] [66040]
Breast Feeding
Ibuprofen is compatible with breast-feeding. Ibuprofen is considered a preferred analgesic or anti-inflammatory agent in lactating individuals. It is present in human milk; however, the amount present is much less than safe doses given to infants.[70364] [70365] Limited published literature reports that orally administered ibuprofen has a relative infant dose (RID) of 0.06% to 0.6% of the breast-feeding individual's weight-adjusted dose.[35893] In a study of milk samples from 13 lactating individuals who took approximately 1,000 mg of ibuprofen daily, the relative infant dose was less than 0.38% of the individual's mean weight-adjusted dose. The relative infant dose was highest when the milk protein content was highest during the colostral phase.[60362]
Interactions
Cidofovir
Ketorolac
Aldesleukin, IL-2
Aspirin, ASA
Bacitracin
Bismuth Subsalicylate
Busulfan
Carmustine, BCNU
Chlorambucil
Cladribine
Cytarabine, ARA-C
Dacarbazine, DTIC
Desmopressin
Diclofenac
Diflunisal
Docetaxel
Enoxaparin
Ethanol
Etodolac
Fenoprofen
Floxuridine
Indomethacin
Ketoprofen
Lomustine, CCNU
Mannitol
Methotrexate
Methoxsalen
Mitoxantrone
Nabumetone
Naproxen
Paclitaxel
Pentamidine
Pentostatin
Piroxicam
Polymyxin B
Probenecid
Procarbazine
Salsalate
Sulindac
Thioguanine, 6-TG
Tolmetin
Celecoxib
Meloxicam
Temozolomide
Acetaminophen; Aspirin, ASA; Caffeine
Aspirin, ASA; Butalbital; Caffeine
Butalbital; Aspirin; Caffeine; Codeine
Aspirin, ASA; Caffeine
Aspirin, ASA; Caffeine; Orphenadrine
Aspirin, ASA; Carisoprodol; Codeine
Aspirin, ASA; Oxycodone
Bismuth Subsalicylate; Metronidazole; Tetracycline
Probenecid; Colchicine
Diclofenac; Misoprostol
Capreomycin
Colistimethate, Colistin, Polymyxin E
Flurbiprofen
Magnesium Salicylate
Oxaprozin
Aminosalicylate sodium, Aminosalicylic acid
Aspirin, ASA; Citric Acid; Sodium Bicarbonate
Aspirin, ASA; Dipyridamole
Naproxen; Pseudoephedrine
Ibritumomab Tiuxetan
Choline Salicylate; Magnesium Salicylate
Eplerenone
Pemetrexed
Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate; Sodium Biphosphate
Clofarabine
Sumatriptan; Naproxen
Nelarabine
Ibuprofen lysine
Dasatinib
Dabigatran
Rivaroxaban
Naproxen; Esomeprazole
Meclofenamate Sodium
Mefenamic Acid
Pralatrexate
Vemurafenib
Benzoic Acid; Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate
Omacetaxine
Apixaban
Edoxaban
Aspirin, ASA; Omeprazole
Diphenhydramine; Naproxen
Macimorelin
Amlodipine; Celecoxib
Pretomanid
Bupivacaine; Meloxicam
Celecoxib; Tramadol
Acetaminophen; Aspirin
Acetaminophen; Aspirin; Diphenhydramine
Methenamine; Sodium Salicylate
Sulopenem Etzadroxil; Probenecid
Meloxicam; Rizatriptan
Colistin
tobacco
Acebutolol
Acyclovir
Alteplase
Amikacin
Amiloride
Amlodipine
Amphotericin B
Atenolol
Auranofin
Azathioprine
Beclomethasone
Benazepril
Betamethasone
Betaxolol
Budesonide
Bumetanide
Captopril
Carbamazepine
Carvedilol
Chlorthalidone
Ciprofloxacin
Cortisone
Cyclosporine
Dalteparin
Dexamethasone
Digoxin
Diltiazem
Dipyridamole
Doxazosin
Enalapril, Enalaprilat
Epoprostenol
Esmolol
Ethacrynic Acid
Felodipine
Fluconazole
Fludrocortisone
Flunisolide
Fluoxetine
Fluticasone
Fluvoxamine
Fosinopril
Furosemide
Gentamicin
Glimepiride
Glipizide
Glyburide
Heparin
Hydrochlorothiazide, HCTZ
Hydrocortisone
Immune Globulin IV, IVIG, IGIV
Indapamide
Isradipine
Labetalol
Levobunolol
Lisinopril
Lithium
Losartan
Methyldopa
Methylprednisolone
Metolazone
Metoprolol
Mifepristone
Moexipril
Nadolol
Neostigmine
Nicardipine
NIFEdipine
Nimodipine
Ofloxacin
Pamidronate
Paroxetine
Phenoxybenzamine
Phentolamine
Physostigmine
Pindolol
Pneumococcal Vaccine, Polyvalent
Potassium Iodide, KI
Prazosin
Prednisolone
Prednisone
Propranolol
Pyridostigmine
Quinapril
Ramipril
Riluzole
Sertraline
Sotalol
Spironolactone
Streptomycin
Tacrolimus
Terazosin
Timolol
Tobramycin
Torsemide
Trazodone
Triamcinolone
Triamterene
Urea
Valacyclovir
Venlafaxine
Verapamil
Warfarin
Anagrelide
Argatroban
Bivalirudin
Citalopram
Clopidogrel
Donepezil
Galantamine
Irbesartan
Leflunomide
Levofloxacin
Pentosan
Reteplase, r-PA
Tirofiban
Trandolapril
Amiloride; Hydrochlorothiazide, HCTZ
Amlodipine; Benazepril
Atenolol; Chlorthalidone
Benazepril; Hydrochlorothiazide, HCTZ
Bisoprolol; Hydrochlorothiazide, HCTZ
Captopril; Hydrochlorothiazide, HCTZ
Potassium Citrate; Citric Acid
Citric Acid; Potassium Citrate; Sodium Citrate
Enalapril; Hydrochlorothiazide, HCTZ
Lisinopril; Hydrochlorothiazide, HCTZ
Losartan; Hydrochlorothiazide, HCTZ
Metoprolol; Hydrochlorothiazide, HCTZ
Spironolactone; Hydrochlorothiazide, HCTZ
Triamterene; Hydrochlorothiazide, HCTZ
Polyethylene Glycol; Electrolytes
Antithrombin III
Bisoprolol
Carteolol
Chlorothiazide
Guanfacine
Mecamylamine
Mometasone
Nisoldipine
Perindopril
Sodium Phosphate Monobasic Monohydrate; Sodium Phosphate Dibasic Anhydrous
Valsartan
Trandolapril; Verapamil
Eptifibatide
Ginkgo, Ginkgo biloba
Adefovir
Aminolevulinic Acid
Candesartan
Cilostazol
Telmisartan
Hydrochlorothiazide, HCTZ; Moexipril
Rivastigmine
Dorzolamide; Timolol
Valsartan; Hydrochlorothiazide, HCTZ
Iodine; Potassium Iodide, KI
Voriconazole
Irbesartan; Hydrochlorothiazide, HCTZ
Tenecteplase
Verteporfin
Emtricitabine
Fluticasone; Salmeterol
Tenofovir Disoproxil Fumarate
Moxifloxacin
Quinapril; Hydrochlorothiazide, HCTZ
Zoledronic Acid
Fosinopril; Hydrochlorothiazide, HCTZ
Glyburide; Metformin
Candesartan; Hydrochlorothiazide, HCTZ
Telmisartan; Hydrochlorothiazide, HCTZ
Duloxetine
Escitalopram
Ibandronate
Fondaparinux
Iloprost
Treprostinil
Olmesartan
Erlotinib
Glipizide; Metformin
Gemifloxacin
Olmesartan; Hydrochlorothiazide, HCTZ
Olanzapine; Fluoxetine
Oritavancin
Ciclesonide
Milnacipran
Potassium Citrate
Amlodipine; Atorvastatin
Iopamidol
Iohexol
Ioversol
Iodixanol
Emtricitabine; Tenofovir Disoproxil Fumarate
Nebivolol
Entecavir
Deferasirox
Prasugrel
Efavirenz; Emtricitabine; Tenofovir Disoproxil Fumarate
Budesonide; Formoterol
Pioglitazone; Glimepiride
Isosulfan Blue
Desvenlafaxine
Aliskiren
Amlodipine; Valsartan
Amlodipine; Olmesartan
Brimonidine; Timolol
Eltrombopag
Aliskiren; Hydrochlorothiazide, HCTZ
Vilazodone
Clevidipine
Amlodipine; Valsartan; Hydrochlorothiazide, HCTZ
Ticagrelor
Amphotericin B lipid complex (ABLC)
Amphotericin B liposomal (LAmB)
Telmisartan; Amlodipine
Formoterol; Mometasone
Olmesartan; Amlodipine; Hydrochlorothiazide, HCTZ
Magnesium Sulfate; Potassium Sulfate; Sodium Sulfate
Azilsartan
Emtricitabine; Rilpivirine; Tenofovir Disoproxil Fumarate
Azilsartan; Chlorthalidone
Azelastine; Fluticasone
Sodium picosulfate; Magnesium oxide; Anhydrous citric acid
Elvitegravir; Cobicistat; Emtricitabine; Tenofovir Disoproxil Fumarate
Fluticasone; Vilanterol
Levomilnacipran
Vortioxetine
Conjugated Estrogens; Bazedoxifene
Vorapaxar
Hyaluronidase, Recombinant; Immune Globulin
Donepezil; Memantine
Perindopril; Amlodipine
Calcium Phosphate, Supersaturated
Sacubitril; Valsartan
Dichlorphenamide
Elvitegravir; Cobicistat; Emtricitabine; Tenofovir Alafenamide
Emtricitabine; Rilpivirine; Tenofovir alafenamide
Emtricitabine; Tenofovir alafenamide
Tenofovir Alafenamide
Deflazacort
Iopromide
Delafloxacin
Fluticasone; Umeclidinium; Vilanterol
Polyethylene Glycol; Electrolytes; Ascorbic Acid
Efavirenz; Lamivudine; Tenofovir Disoproxil Fumarate
Bictegravir; Emtricitabine; Tenofovir Alafenamide
Lamivudine; Tenofovir Disoproxil Fumarate
Darunavir; Cobicistat; Emtricitabine; Tenofovir alafenamide
Potassium Chloride
Potassium Acetate
Potassium Bicarbonate
Potassium Gluconate
Doravirine; Lamivudine; Tenofovir disoproxil fumarate
Inotersen
Pexidartinib
Levamlodipine
Ethiodized Oil
Budesonide; Glycopyrrolate; Formoterol
Sodium Sulfate; Magnesium Sulfate; Potassium Chloride
Voclosporin
Olopatadine; Mometasone
Iomeprol
Albuterol; Budesonide
Sparsentan
Neostigmine; Glycopyrrolate
Fidanacogene Elaparvovec
Benzgalantamine
Landiolol
Gepotidacin
Alpha-blockers
Corticosteroids
Quinolones
Thrombolytic Agents
Platelet Inhibitors
Thiazide diuretics
Cardiac glycosides
Selective serotonin reuptake inhibitors
Beta-blockers
Sulfonylureas
Angiotensin II receptor antagonists
Potassium
Angiotensin-converting enzyme inhibitors
Photosensitizing agents (topical)
Calcium-channel blockers
Cholinesterase inhibitors
Gold
Non-Ionic Contrast Media
Ionic Contrast Media
Alendronate
Cefotaxime
Cholestyramine
Foscarnet
Ganciclovir
Mesalamine, 5-ASA
Neomycin
Vancomycin
Zafirlukast
Ginger, Zingiber officinale
Risedronate
Garlic, Allium sativum
Valganciclovir
Drospirenone; Ethinyl Estradiol
Aprepitant, Fosaprepitant
Alendronate; Cholecalciferol
Telavancin
Drospirenone; Estradiol
Fenofibric Acid
Levomefolate
Drospirenone; Ethinyl Estradiol; Levomefolate
Ivacaftor
Lumacaftor; Ivacaftor
Tezacaftor; Ivacaftor
Drospirenone
Elexacaftor; tezacaftor; ivacaftor
Drospirenone; Estetrol
Lumacaftor; Ivacaftor
Acebutolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Acetaminophen; Aspirin, ASA; Caffeine: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Acetaminophen; Aspirin: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Acetaminophen; Aspirin; diphenhydrAMINE: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Acyclovir: (Moderate) Monitor patients for signs of worsening renal function during coadministration of acyclovir and nonsteroidal antiinflammatory drugs. Coadministration may increase the risk for drug-induced nephrotoxicity. [34408] [56268]
Adefovir: (Moderate) Chronic coadministration of adefovir with nephrotoxic drugs, such as nonsteroidal antiinflammatory drugs may increase the risk of developing nephrotoxicity even in patients who have normal renal function. The use of adefovir with NSAIDs may be done cautiously. As stated in the current adefovir prescribing information, 'Ibuprofen (800 mg PO three times daily), when given concomitantly with adefovir dipivoxil, increased the adefovir Cmax by 33% and AUC by 23%, as well as urinary recovery. The increase appears to be due to higher oral bioavailability, not a reduction in renal clearance of adefovir.' In an in vitro investigation, the antiviral effect of adefovir was unaltered and the renal proximal tubule accumulation of adefovir was inhibited by the presence of a NSAID. Adefovir is efficiently transported by the human renal organic anion transporter 1, and the presence of this transporter appears to mediate the accumulation of the drug in renal proximal tubules. The in vitro study suggests that the use of a NSAID with adefovir may potentially reduce the nephrotoxic potential of adefovir. Of course, NSAIDs are associated with nephrotoxicity of their own; therefore, further data on the interaction between NSAIDs and adefovir in humans are needed. [27615]
Albuterol; Budesonide: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Aldesleukin, IL-2: (Major) Aldesleukin, IL-2 may cause nephrotoxicity. Concurrent administration of drugs possessing nephrotoxic effects, such as nonsteroidal antiinflammatory agents (NSAIDs), with Aldesleukin, IL-2 may increase the risk of kidney dysfunction. In addition, reduced kidney function secondary to Aldesleukin, IL-2 treatment may delay elimination of concomitant medications and increase the risk of adverse events from those drugs. [41853]
Alendronate: (Minor) Monitor for gastrointestinal adverse events during concurrent use of alendronate and nonsteroidal antiinflammatory drugs. Both medications have been associated with gastrointestinal irritation although data suggest concomitant use introduces little additional risk for adverse effects for most patients. [28644] [52249]
Alendronate; Cholecalciferol: (Minor) Monitor for gastrointestinal adverse events during concurrent use of alendronate and nonsteroidal antiinflammatory drugs. Both medications have been associated with gastrointestinal irritation although data suggest concomitant use introduces little additional risk for adverse effects for most patients. [28644] [52249]
Aliskiren: (Moderate) NSAIDs may attenuate the antihypertensive effects of aliskiren by inhibiting the synthesis of vasodilatory prostaglandins. In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function who are being treated with NSAIDs, the coadministration of aliskiren may result in a further deterioration of renal function, including acute renal failure. These effects are usually reversible. Therefore, blood pressure and renal function should be monitored closely when an NSAID is administered to a patient taking aliskiren. [30489] [33200]
Aliskiren; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) NSAIDs may attenuate the antihypertensive effects of aliskiren by inhibiting the synthesis of vasodilatory prostaglandins. In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function who are being treated with NSAIDs, the coadministration of aliskiren may result in a further deterioration of renal function, including acute renal failure. These effects are usually reversible. Therefore, blood pressure and renal function should be monitored closely when an NSAID is administered to a patient taking aliskiren. [30489] [33200]
Alpha-blockers: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Alteplase: (Moderate) NSAIDs can cause GI bleeding, inhibit platelet aggregation, prolong bleeding time; these pharmacodynamic effects may be increased when administered to patients receiving thrombolytic agents. Patients receiving these drugs concurrently should be monitored closely for bleeding. [28469] [30569]
Amikacin: (Moderate) It is possible that additive nephrotoxicity may occur in patients who receive nonsteroidal antiinflammatory drugs (NSAIDs) concurrently with other nephrotoxic agents, such as amikacin. [28370] [30110] [30268]
aMILoride: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the natriuretic effect of diuretics in some patients. NSAIDS have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. Patients taking diuretics and NSAIDS concurrently are at higher risk of developing renal insufficiency. If an NSAID and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. [30489] [48492]
aMILoride; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the natriuretic effect of diuretics in some patients. NSAIDS have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. Patients taking diuretics and NSAIDS concurrently are at higher risk of developing renal insufficiency. If an NSAID and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. [30489] [48492]
Aminolevulinic Acid: (Moderate) Agents that inhibit prostaglandin synthesis such as nonsteroidal antiinflammatory drugs (NSAIDs), could decrease the efficacy of photosensitizing agents used in photodynamic therapy. Avoidance of NSAIDs before and during photodynamic therapy may be advisable. [42968]
Aminosalicylate sodium, Aminosalicylic acid: (Major) Avoid concomitant use of ibuprofen with aminosalicylic acid due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
amLODIPine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
amLODIPine; Atorvastatin: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
amLODIPine; Benazepril: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
amLODIPine; Celecoxib: (Major) Avoid concomitant use of celecoxib with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [28317] [35893] (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
amLODIPine; Olmesartan: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
amLODIPine; Valsartan: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
amLODIPine; Valsartan; hydroCHLOROthiazide, HCTZ: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Amphotericin B lipid complex (ABLC): (Moderate) Concurrent use of amphotericin B and other nephrotoxic medications, including nonsteroidal antiinflammatory drugs (NSAIDs), may enhance the potential for drug-induced renal toxicity. Monitor renal function carefully during concurrent therapy. Amphotericin B dosage reduction may be necessary if renal impairment occurs. [28333] [30268]
Amphotericin B liposomal (LAmB): (Moderate) Concurrent use of amphotericin B and other nephrotoxic medications, including nonsteroidal antiinflammatory drugs (NSAIDs), may enhance the potential for drug-induced renal toxicity. Monitor renal function carefully during concurrent therapy. Amphotericin B dosage reduction may be necessary if renal impairment occurs. [28333] [30268]
Amphotericin B: (Moderate) Concurrent use of amphotericin B and other nephrotoxic medications, including nonsteroidal antiinflammatory drugs (NSAIDs), may enhance the potential for drug-induced renal toxicity. Monitor renal function carefully during concurrent therapy. Amphotericin B dosage reduction may be necessary if renal impairment occurs. [28333] [30268]
Anagrelide: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Angiotensin II receptor antagonists: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Angiotensin-converting enzyme inhibitors: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Antithrombin III: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal anti-inflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Apixaban: (Major) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [52739]
Aprepitant, Fosaprepitant: (Minor) Use caution if ibuprofen and aprepitant are used concurrently and monitor for a possible decrease in the efficacy of ibuprofen. After administration, fosaprepitant is rapidly converted to aprepitant and shares the same drug interactions. Ibuprofen is a CYP2C9 substrate and aprepitant is a CYP2C9 inducer. Administration of a CYP2C9 substrate, tolbutamide, on days 1, 4, 8, and 15 with a 3-day regimen of oral aprepitant (125 mg/80 mg/80 mg) decreased the tolbutamide AUC by 23% on day 4, 28% on day 8, and 15% on day 15. The AUC of tolbutamide was decreased by 8% on day 2, 16% on day 4, 15% on day 8, and 10% on day 15 when given prior to oral administration of aprepitant 40 mg on day 1, and on days 2, 4, 8, and 15. The effects of aprepitant on tolbutamide were not considered significant. When a 3-day regimen of aprepitant (125 mg/80 mg/80 mg) given to healthy patients on stabilized chronic warfarin therapy (another CYP2C9 substrate), a 34% decrease in S-warfarin trough concentrations was noted, accompanied by a 14% decrease in the INR at five days after completion of aprepitant. [30676] [34453] [34454] [34462] [40027]
Argatroban: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal anti-inflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Aspirin, ASA: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; Butalbital; Caffeine: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; Caffeine: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; Caffeine; Orphenadrine: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; Carisoprodol; Codeine: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; Citric Acid; Sodium Bicarbonate: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; Dipyridamole: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171] (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Aspirin, ASA; Omeprazole: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Aspirin, ASA; oxyCODONE: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Atenolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Atenolol; Chlorthalidone: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Auranofin: (Moderate) Due to the inhibition of renal prostaglandins by NSAIDs, concurrent use with other nephrotoxic agents, such as gold compounds, may lead to additive nephrotoxicity. Monitor renal function carefully during concurrent therapy. [30110] [30268]
azaTHIOprine: (Moderate) NSAIDs should be used with caution in patients receiving immunosuppressives as they may mask fever, pain, swelling and other signs and symptoms of an infection. [6144]
Azelastine; Fluticasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Azilsartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Azilsartan; Chlorthalidone: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Bacitracin: (Major) Avoid concurrent use of bacitracin with nonsteroidal antiinflammatory drugs. Coadministration may increase the risk for drug-induced nephrotoxicity. [31047] [56268]
Beclomethasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Benazepril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Benazepril; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Benzgalantamine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Benzoic Acid; Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate: (Major) Avoid concomitant use of ibuprofen with phenyl salicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Beta-blockers: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Betamethasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Betaxolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Bictegravir; Emtricitabine; Tenofovir Alafenamide: (Moderate) Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) and tenofovir alafenamide may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [61413] [71829] [72477] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Bismuth Subsalicylate: (Major) Avoid concomitant use of ibuprofen with bismuth subsalicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Bismuth Subsalicylate; metroNIDAZOLE; Tetracycline: (Major) Avoid concomitant use of ibuprofen with bismuth subsalicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Bisoprolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Bisoprolol; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Bivalirudin: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal anti-inflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Brimonidine; Timolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Budesonide: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Budesonide; Formoterol: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Budesonide; Glycopyrrolate; Formoterol: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Bumetanide: (Moderate) If a nonsteroidal anti-inflammatory drug (NSAID) and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. Patients taking diuretics and NSAIDs concurrently are at higher risk of developing renal insufficiency. NSAIDs may reduce the natriuretic effect of diuretics in some patients. NSAIDs have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. [30489] [48492]
BUPivacaine; Meloxicam: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [29611] [35893]
Busulfan: (Major) Due to the thrombocytopenic effects of busulfan, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, ASA, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [4736] [5170]
Butalbital; Aspirin; Caffeine; Codeine: (Major) Concomitant use of analgesic doses of aspirin and ibuprofen is generally not recommended due to the increased risk of bleeding and renal impairment. Because there may be an increased risk of cardiovascular events due to the interference of ibuprofen with the antiplatelet effect of aspirin, for patients taking low-dose aspirin for cardioprotection who require analgesics, consider use of an NSAID that does not interfere with the antiplatelet effect of aspirin, or non-NSAID analgesics, as appropriate. Administer single doses of ibuprofen at least 2 to 4 hours or more after aspirin and wait 8 hours after ibuprofen administration before administering aspirin to avoid significant interference. Monitor for signs and symptoms of renal impairment. Pharmacodynamic studies have demonstrated interference with the antiplatelet activity of aspirin when ibuprofen 400 mg 3 times daily is administered with enteric-coated low-dose aspirin. The interaction exists even after ibuprofen 400 mg once daily, particularly when ibuprofen is dosed prior to aspirin. The interaction is alleviated if immediate-release low-dose aspirin is dosed at least 2 hours prior to a once daily regimen of ibuprofen; however, this finding cannot be extended to enteric-coated low-dose aspirin. A decrease in antiplatelet activity (53%) was observed when ibuprofen 400 mg once daily was administered 2 hours before low-dose immediate-release aspirin 81 mg/day for 6 days. An interaction was still observed, but minimized, when ibuprofen 400 mg once daily was administered as early as 8 hours before immediate-release aspirin (90.7%). There was no interaction with the antiplatelet activity of aspirin when ibuprofen 400 mg once daily was administered 2 hours after immediate-release aspirin (99.2%). In another study of low-dose immediate-release aspirin 81 mg/day and ibuprofen 400 mg 3 times daily (1, 7, and 13 hours post-aspirin dose) for 10 consecutive days, there was no interaction with the antiplatelet activity of aspirin (98.3%); however, there were individuals with aspirin antiplatelet activity below 95%, with the lowest being 90.2%. When a similarly designed study was conducted with enteric-coated aspirin 81 mg/day for 6 days and ibuprofen 400 mg 3 times daily (2, 7 and 12 h post-aspirin dose) for 6 days, there was an interaction with the antiplatelet activity at 24 hours after the day 6 aspirin dose (67%). Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone. Ibuprofen is not a substitute for low dose aspirin for cardiovascular protection. [35893] [60438] [61171]
Calcium Phosphate, Supersaturated: (Moderate) Concomitant use of medicines with potential to alter renal perfusion or function such as nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk of acute phosphate nephropathy in patients taking sodium phosphate monobasic monohydrate; sodium phosphate dibasic anhydrous. [32159] [32160]
Calcium-channel blockers: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Candesartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Candesartan; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Capreomycin: (Major) Because capreomycin is primarily eliminated by the kidney, coadministration with other potentially nephrotoxic drugs, including nonsteroidal antiinflammatory drugs (NSAIDs), may increase serum concentrations of either drug. Theoretically, the chronic coadministration of these drugs may increase the risk of developing nephrotoxicity, even in patients who have normal renal function. Monitor patients for changes in renal function if these drugs are coadministered. [44155]
Captopril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Captopril; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
carBAMazepine: (Moderate) Monitor carbamazepine concentrations closely during coadministration of ibuprofen; carbamazepine dose adjustments may be needed. Concomitant use may increase carbamazepine concentrations. [28024] [41237]
Cardiac glycosides: (Moderate) Monitor for signs and symptoms of digoxin toxicity during concomitant ibuprofen use. A decline in GFR or tubular secretion, as from nonsteroidal anti-inflammatory drugs (NSAIDs), may impair the excretion of digoxin. [28272]
Carmustine, BCNU: (Major) Due to the thrombocytopenic effects of carmustine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, ASA, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. These additive effects may not occur for at least 6 weeks after the administration of carmustine due to the delayed myelosuppressive effects of carmustine. [5170] [5946]
Carteolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Carvedilol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Cefotaxime: (Minor) Cefotaxime's product label states that cephalosporins may potentiate the adverse renal effects of nephrotoxic agents, such as aminoglycosides, nonsteroidal antiinflammatory drugs (NSAIDs), and loop diuretics. Carefully monitor renal function, especially during prolonged therapy or use of high aminoglycoside doses. The majority of reported cases involve the combination of aminoglycosides and cephalothin or cephaloridine, which are associated with dose-related nephrotoxicity as singular agents. Limited but conflicting data with other cephalosporins have been noted. [28646] [29912] [57694] [57695] [58208]
Celecoxib: (Major) Avoid concomitant use of celecoxib with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [28317] [35893]
Celecoxib; Tramadol: (Major) Avoid concomitant use of celecoxib with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [28317] [35893]
Chlorambucil: (Major) Due to the thrombocytopenic effects of chlorambucil, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, ASA, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [4757] [5170]
Chlorothiazide: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Chlorthalidone: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Cholestyramine: (Minor) As with other nonsteroidal anti-inflammatory drugs (NSAIDs), the absorption of ibuprofen can be delayed if cholestyramine is concomitantly administered. Staggering the administration times may minimize this interaction. [44130]
Choline Salicylate; Magnesium Salicylate: (Major) Avoid concomitant use of ibuprofen with choline salicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171] (Major) Avoid concomitant use of ibuprofen with magnesium salicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Cholinesterase inhibitors: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Ciclesonide: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Cidofovir: (Contraindicated) The concomitant administration of cidofovir and nonsteroidal antiinflammatory drugs (NSAIDs) is contraindicated due to the potential for increased nephrotoxicity. NSAIDs should be discontinued 7 days prior to beginning cidofovir. [28388]
Cilostazol: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Ciprofloxacin: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
Citalopram: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Citric Acid; Potassium Citrate; Sodium Citrate: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Cladribine: (Major) Due to the thrombocytopenic effects of cladribine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [7226]
Clevidipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Clofarabine: (Major) Due to the thrombocytopenic effects of clofarabine, an additive risk of bleeding may be seen in patients receiving concomitant NSAIDs. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [7557]
Clopidogrel: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Colistimethate, Colistin, Polymyxin E: (Major) The administration of colistimethate sodium may increase the risk of developing nephrotoxicity, even in patients who have normal renal function. Nonsteroidal antiinflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when used concurrently. Monitor patients for changes in renal function if these drugs are coadministered. Since colistimethate sodium is eliminated by the kidney, coadministration with other potentially nephrotoxic drugs, including nonsteroidal antiinflammatory drugs (NSAIDs), may theoretically increase serum concentrations of either drug. [33636]
Colistin: (Major) The administration of colistimethate sodium may increase the risk of developing nephrotoxicity, even in patients who have normal renal function. Nonsteroidal antiinflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when used concurrently. Monitor patients for changes in renal function if these drugs are coadministered. Since colistimethate sodium is eliminated by the kidney, coadministration with other potentially nephrotoxic drugs, including nonsteroidal antiinflammatory drugs (NSAIDs), may theoretically increase serum concentrations of either drug. [33636]
Conjugated Estrogens; Bazedoxifene: (Moderate) In clinical evaluation, a single dose of ibuprofen 600 mg was given with a bazedoxifene 20 mg capsule in 12 postmenopausal women after an overnight fast. Co-administration increased the Cmax and AUC of bazedoxifene by 18% and 7%, respectively. The Cmax of ibuprofen increased by 6%, the AUC was unchanged. The clinical effect of this change is not known. However, co-administration of ibuprofen and conjugated estrogens; bazedoxifene may increase bazedoxifene efficacy and/or side effects. Use caution during coadministration and monitor patient closely. [56074]
Corticosteroids: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Cortisone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
cycloSPORINE: (Moderate) Serum creatinine, potassium concentrations, and cyclosporine concentrations should be closely monitored when systemic cyclosporine is given with nonsteroidal antiinflammatory drugs (NSAIDs). Renal dysfunction associated with cyclosporine may be potentiated by concurrent usage of NSAIDs. The effects of NSAIDs on the production of renal prostaglandins may cause changes in the elimination of cyclosporine. Potentiation of renal dysfunction may especially occur in a dehydrated patient. Patients should be monitored for signs and symptoms of cyclosporine toxicity and infection, as NSAIDs may mask fever, pain, or swelling. Increased tear production was not seen in patients receiving ophthalmic NSAIDs or using punctual plugs concurrently with cyclosporine ophthalmic emulsion. [29198] [30496]
Cytarabine, ARA-C: (Major) The main toxic effect of cytarabine, ARA-C is bone marrow suppression with leukopenia, thrombocytopenia and anemia. Due to the thrombocytopenic effects of cytarabine, an additive risk of bleeding may be seen in patients receiving concomitant NSAIDs. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. Dipyridamole can block membrane transport of cytarabine in tumor cells, therefore decreasing its antineoplastic activity. [5170] [7945]
Dabigatran: (Major) Educate patients about the signs of increased bleeding and the need to report these signs to a healthcare provider immediately if coadministration of dabigatran and a nonsteroidal antiinflammatory drug (NSAID) is necessary. Dabigatran can cause significant and, sometimes, fatal bleeding. This risk may be increased by concurrent use of chronic NSAID therapy. [42121]
Dacarbazine, DTIC: (Major) Leukopenia and thrombocytopenia are common toxicities of dacarbazine, DTIC. Due to the thrombocytopenic effects of dacarbazine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, ASA, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [7996]
Dalteparin: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Darunavir; Cobicistat; Emtricitabine; Tenofovir alafenamide: (Moderate) Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) and tenofovir alafenamide may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [61413] [71829] [72477] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Dasatinib: (Major) Due to the thrombocytopenic and possible platelet inhibiting effects of dasatinib, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors (including aspirin), strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. Caution should be exercised if patients are required to take medications that inhibit platelet function or anticoagulants concomitantly with dasatinib. [32387] [5170]
Deferasirox: (Moderate) Because gastric ulceration and GI bleeding have been reported in patients taking deferasirox, use caution when coadministering with other drugs known to increase the risk of peptic ulcers or gastric hemorrhage including NSAIDs. In addition, coadministration of deferasirox with other potentially nephrotoxic drugs, including NSAIDs, may increase the acute renal failure. Monitor serum creatinine and/or creatinine clearance in patients who are receiving deferasirox and nephrotoxic drugs concomitantly. [31807]
Deflazacort: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Delafloxacin: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
Desmopressin: (Major) Additive hyponatremic effects may be seen in patients treated with desmopressin and drugs associated with hyponatremia including NSAIDs. Use combination with caution, and monitor patients for signs and symptoms of hyponatremia. A woman who took both desmopressin and ibuprofen was found in a comatose state. As her serum sodium concentration was 121 mmol/L, and her plasma osmolality was low in the presence of a high-normal urine osmolality and normal sodium excretion, she was treated with fluid restriction. Her serum sodium concentration was 124 mmol/L within a day and was 135 mmol/L by the second day. The woman had previously received desmopressin without the development of clinical symptoms of hyponatremia. [10457] [10458] [29202]
Desvenlafaxine: (Moderate) Platelet aggregation may be impaired by desvenlafaxine due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Patients should be monitored for signs and symptoms of bleeding while taking desvenlafaxine with NSAIDs. [28275] [29934]
dexAMETHasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Dichlorphenamide: (Moderate) Use dichlorphenamide and ibuprofen together with caution as both drugs can cause metabolic acidosis. Concurrent use may increase the severity of metabolic acidosis. Measure sodium bicarbonate concentrations at baseline and periodically during dichlorphenamide treatment. If metabolic acidosis occurs or persists, consider reducing the dose or discontinuing dichlorphenamide therapy. [44120] [44121] [60122]
Diclofenac: (Major) Avoid concomitant use of diclofenac with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30115] [35893]
Diclofenac; miSOPROStol: (Major) Avoid concomitant use of diclofenac with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30115] [35893]
Diflunisal: (Major) Avoid concomitant use of diflunisal with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [35893] [49143]
Digoxin: (Moderate) Monitor for signs and symptoms of digoxin toxicity during concomitant ibuprofen use. A decline in GFR or tubular secretion, as from nonsteroidal anti-inflammatory drugs (NSAIDs), may impair the excretion of digoxin. [28272]
dilTIAZem: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
diphenhydrAMINE; Naproxen: (Major) Avoid concomitant use of ibuprofen with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [32122] [35893]
Dipyridamole: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
DOCEtaxel: (Major) Due to the thrombocytopenic effects of docetaxel, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors (including aspirin), strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [5235]
Donepezil: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Donepezil; Memantine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Doravirine; lamiVUDine; Tenofovir disoproxil fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268]
Dorzolamide; Timolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Doxazosin: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Drospirenone: (Minor) Drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium. Other drugs that may have additive effects on serum potassium with drospirenone include chronic treatment with NSAIDs, and monitoring of serum potassium in the 1st month of concurrent therapy is recommended. [4716]
Drospirenone; Estetrol: (Minor) Drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium. Other drugs that may have additive effects on serum potassium with drospirenone include chronic treatment with NSAIDs, and monitoring of serum potassium in the 1st month of concurrent therapy is recommended. [4716]
Drospirenone; Estradiol: (Minor) Drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium. Other drugs that may have additive effects on serum potassium with drospirenone include chronic treatment with NSAIDs, and monitoring of serum potassium in the 1st month of concurrent therapy is recommended. [4716]
Drospirenone; Ethinyl Estradiol: (Minor) Drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium. Other drugs that may have additive effects on serum potassium with drospirenone include chronic treatment with NSAIDs, and monitoring of serum potassium in the 1st month of concurrent therapy is recommended. [4716]
Drospirenone; Ethinyl Estradiol; Levomefolate: (Minor) Drospirenone has antimineralocorticoid effects; the progestin may increase serum potassium. Other drugs that may have additive effects on serum potassium with drospirenone include chronic treatment with NSAIDs, and monitoring of serum potassium in the 1st month of concurrent therapy is recommended. [4716] (Minor) L-methylfolate should be used cautiously in patients taking high doses of ibuprofen. Plasma concentrations of L-methylfolate may be reduced when used concomitantly with high doses of ibuprofen. Monitor patients for decreased efficacy of L-methylfolate if these agents are used together. [35581]
DULoxetine: (Moderate) Monitor for signs and symptoms of bleeding during concomitant duloxetine and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [29934]
Edoxaban: (Major) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Efavirenz; Emtricitabine; Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Efavirenz; lamiVUDine; Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268]
Elexacaftor; tezacaftor; ivacaftor: (Minor) Increased monitoring is recommended if ivacaftor is administered concurrently with CYP2C9 substrates, such as ibuprofen. In vitro studies showed ivacaftor to be a weak inhibitor of CYP2C9. Co-administration may lead to increased exposure to CYP2C9 substrates; however, the clinical impact of this has not yet been determined. [48524]
Eltrombopag: (Moderate) Eltrombopag is a UDP-glucuronyltransferase inhibitor. NSAIDs are a substrate of UDP-glucuronyltransferases. The significance or effect of this interaction is not known; however, elevated concentrations of the NSAID are possible. Monitor patients for adverse reactions if eltrombopag is administered with an NSAID. [40392]
Elvitegravir; Cobicistat; Emtricitabine; Tenofovir Alafenamide: (Moderate) Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) and tenofovir alafenamide may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [61413] [71829] [72477] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014] (Moderate) The plasma concentrations of ibuprofen may be decreased when administered concurrently with elvitegravir. Patients may experience decreased analgesic or anti-inflammatory effects when these drugs are coadministered. Elvitegravir is a CYP2C9 inducer, while ibuprofen is a CYP2C9 substrate. [34454] [51664] [58001]
Elvitegravir; Cobicistat; Emtricitabine; Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014] (Moderate) The plasma concentrations of ibuprofen may be decreased when administered concurrently with elvitegravir. Patients may experience decreased analgesic or anti-inflammatory effects when these drugs are coadministered. Elvitegravir is a CYP2C9 inducer, while ibuprofen is a CYP2C9 substrate. [34454] [51664] [58001]
Emtricitabine: (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Emtricitabine; Rilpivirine; Tenofovir alafenamide: (Moderate) Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) and tenofovir alafenamide may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [61413] [71829] [72477] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Emtricitabine; Rilpivirine; Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Emtricitabine; Tenofovir alafenamide: (Moderate) Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) and tenofovir alafenamide may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [61413] [71829] [72477] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Emtricitabine; Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268] (Moderate) Monitor for nonsteroidal antiinflammatory drug (NSAID) or emtricitabine-related adverse events during concomitant use. Concomitant use may increase NSAID or emtricitabine concentrations. Coadministration of drugs that reduce renal function or compete for active tubular secretion, such as NSAIDs and emtricitabine, may increase the risk of adverse reactions. [35893] [51664] [64014]
Enalapril, Enalaprilat: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Enalapril; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Enoxaparin: (Major) Whenever possible, discontinue agents which may enhance the risk of hemorrhage, including nonsteroidal antiinflammatory drugs, before initiation of enoxaparin therapy. If coadministration is essential, conduct close clinical and laboratory monitoring. [29732]
Entecavir: (Moderate) The manufacturer of entecavir recommends monitoring for adverse effects when coadministered with NSAIDs. Entecavir is primarily eliminated by the kidneys; NSAIDs can affect renal function. Concurrent administration may increase the serum concentrations of entecavir and adverse events. [31230]
Eplerenone: (Major) Monitor serum potassium and serum creatinine concentrations within 3 to 7 days of initiating coadministration of eplerenone and nonsteroidal antiinflammatory drugs (NSAIDs), and monitor blood pressure. The concomitant use of other potassium-sparing antihypertensives with NSAIDs has been shown to reduce the antihypertensive effect in some patients and result in severe hyperkalemia in patients with impaired renal function. Patients who develop hyperkalemia may continue eplerenone with proper dose adjustment; eplerenone dose reduction decreases potassium concentrations. [27990]
Epoprostenol: (Moderate) NSAIDs may decrease the effect of antihypertensive agents through various mechanisms, including renal and peripheral vasoactive pathways. [4087]
Eptifibatide: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Erlotinib: (Moderate) Monitor for symptoms of gastrointestinal (GI) perforation (e.g., severe abdominal pain, fever, nausea, and vomiting) if coadministration of erlotinib with nonsteroidal antiinflammatory drugs (NSAIDs) is necessary. Permanently discontinue erlotinib in patients who develop GI perforation. The pooled incidence of GI perforation clinical trials of erlotinib ranged from 0.1% to 0.4%, including fatal cases. Patients receiving concomitant NSAIDs may be at increased risk of perforation. [30555]
Escitalopram: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Esmolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Ethacrynic Acid: (Moderate) If a nonsteroidal anti-inflammatory drug (NSAID) and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. Patients taking diuretics and NSAIDs concurrently are at higher risk of developing renal insufficiency. NSAIDs may reduce the natriuretic effect of diuretics in some patients. NSAIDs have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. [30489] [48492]
Ethanol: (Major) Advise patients to avoid alcohol and alcohol-containing products while taking NSAIDs. Concomitant ingestion of alcohol with NSAIDs increases the risk of developing gastric irritation and GI mucosal bleeding. Alcohol is a mucosal irritant and NSAIDs decrease platelet aggregation. Routine ingestion of alcohol and NSAIDs can cause significant GI bleeding, which may or may not be overt. Even occasional concomitant use of NSAIDs and alcohol should be avoided. Chronic alcohol ingestion is often associated with hypoprothrombinemia and this condition increases the risk of bleeding. [30115] [30427] [30569] [31949]
Ethiodized Oil: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Etodolac: (Major) Avoid concomitant use of etodolac with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [35893] [45875]
Felodipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Fenofibric Acid: (Minor) At therapeutic concentrations, fenofibric acid is a mild-to-moderate inhibitor of CYP2C9. Concomitant use of fenofibric acid with CYP2C9 substrates, such as ibuprofen, has not been formally studied. Fenofibric acid may theoretically increase plasma concentrations of CYP2C9 substrates and could lead to toxicity for drugs that have a narrow therapeutic range. Monitor the therapeutic effect of ibuprofen during coadministration with fenofibric acid. [11310] [11311] [11319] [49952]
Fenoprofen: (Major) Avoid concomitant use of fenoprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30524] [35893]
Fidanacogene Elaparvovec: (Moderate) Monitor for hepatoxicity during concomitant use of fidanacogene elaparvovec and ibuprofen. Both medications have been associated with hepatic injury and concomitant use may increase the risk for hepatotoxicity. Hepatic injury may also lead to decreased fidanacogene elaparvovec efficacy. [63549] [70571]
Floxuridine: (Major) Due to the thrombocytopenic effects of floxuridine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [7446]
Fluconazole: (Moderate) Fluconazole is an inhibitor of CYP2C9, which is the isoenzyme responsible for the metabolism of ibuprofen. Thus, increased plasma concentrations of ibuprofen are possible. If fluconazole is administered concurrently with ibuprofen, monitor for NSAID-related side-effects such as fluid retention, GI irritation, or renal dysfunction and adjust the ibuprofen dose, if needed. Among 12 healthy males, the mean systemic exposure of S-(+)-ibuprofen after a single dose of 400 mg of racemic ibuprofen was 67.4 +/- 16.2 mcg x hour/mL. In contrast, the mean systemic exposure was 122 +/- 32 mcg x hour/mL when ibuprofen was given 1 hour after the second fluconazole dose; fluconazole 400 mg was given on day 1 and 200 mg was given on day 2. In addition to increased systemic exposure, the maximum concentration and half-life of S-(+)-ibuprofen were all statistically significantly greater in the presence of fluconazole. Increased S-(+)-ibuprofen concentrations leads to increased inhibition of both COX-1 and COX-2, and impaired ibuprofen metabolism due to mutations in the CYP2C9 gene increases the risk of acute gastrointestinal bleeding. [29036] [34447] [34453] [34454] [34461]
Fludrocortisone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Flunisolide: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
FLUoxetine: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Flurbiprofen: (Major) Avoid concomitant use of flurbiprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30241] [35893]
Fluticasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Fluticasone; Salmeterol: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Fluticasone; Umeclidinium; Vilanterol: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Fluticasone; Vilanterol: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
fluvoxaMINE: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Fondaparinux: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Formoterol; Mometasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Foscarnet: (Minor) The risk of renal toxicity may be increased if foscarnet is used in conjuction with other nephrotoxic agents, such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor renal function carefully during concurrent therapy. [28377] [30268]
Fosinopril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Fosinopril; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Furosemide: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant furosemide and ibuprofen use. Nonsteroidal antiinflammatory drugs (NSAIDs) may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of loop diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Galantamine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Ganciclovir: (Minor) Concurrent use of nephrotoxic agents, such as NSAIDs, with ganciclovir should be done cautiously to avoid additive nephrotoxicity. Monitor renal function carefully if concomitant therapy is required. [32676]
Garlic, Allium sativum: (Minor) Garlic, Allium sativum may produce clinically-significant antiplatelet effects; until more data are available, garlic should be used cautiously in patients receiving drugs with a known potential risk for bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). [25588] [63043]
Gemifloxacin: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
Gentamicin: (Moderate) It is possible that additive nephrotoxicity may occur in patients who receive nonsteroidal anti-inflammatory drugs (NSAIDs) concurrently with other nephrotoxic agents, such as gentamicin. [28370] [30110] [30268]
Gepotidacin: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Ginger, Zingiber officinale: (Minor) Patients receiving regular therapy with nonsteroidal antiinflammatory drugs (NSAIDs) should use ginger with caution, due to a theoretical risk of bleeding resulting from additive pharmacology related to the COX enzymes. However, clinical documentation of interactions is lacking. Several pungent constituents of ginger (Zingiber officinale) are reported to inhibit arachidonic acid (AA) induced platelet activation in human whole blood. The constituent (8)-paradol is the most potent inhibitor of COX-1 and exhibits the greatest anti-platelet activity versus other gingerol analogues. The mechanism of ginger-associated platelet inhibition may be related to decreased COX-1/Thomboxane synthase enzymatic activity. [28470] [29960]
Ginkgo, Ginkgo biloba: (Moderate) Monitor for signs or symptoms of bleeding with coadministration of ginkgo biloba and NSAIDs as an increased bleeding risk may occur. Although data are mixed, ginkgo biloba is reported to inhibit platelet aggregation and several case reports describe bleeding complications with ginkgo biloba, with or without concomitant drug therapy. [25082] [25083] [25273] [28470] [41251] [41258] [41265]
Glimepiride: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
glipiZIDE: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
glipiZIDE; metFORMIN: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
glyBURIDE: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
glyBURIDE; metFORMIN: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
Gold: (Moderate) Due to the inhibition of renal prostaglandins by NSAIDs, concurrent use with other nephrotoxic agents, such as gold compounds, may lead to additive nephrotoxicity. Monitor renal function carefully during concurrent therapy. [30110] [30268]
guanFACINE: (Moderate) NSAIDs may decrease the effect of antihypertensive agents through various mechanisms, including renal and peripheral vasoactive pathways. [805]
Heparin: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Hyaluronidase, Recombinant; Immune Globulin: (Moderate) Immune Globulin (IG) products have been reported to be associated with renal dysfunction, acute renal failure, osmotic nephrosis, and death. Patients predisposed to acute renal failure include patients receiving known nephrotoxic drugs like nonsteroidal anti-inflammatory drugs (NSAIDs) and salicylates. Coadminister IG products at the minimum concentration available and the minimum rate of infusion practicable. Also, closely monitor renal function. [6859] [7020] [7823]
hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
hydroCHLOROthiazide, HCTZ; Moexipril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Hydrocortisone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Hyoscyamine; Methenamine; Methylene Blue; Phenyl Salicylate; Sodium Biphosphate: (Major) Avoid concomitant use of ibuprofen with phenyl salicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Ibandronate: (Moderate) Monitor renal function and for gastrointestinal adverse events during concurrent use of intravenous or oral ibandronate, respectively, and nonsteroidal antiinflammatory drugs. Acute renal failure has been observed with intravenous ibandronate and concomitant use of other nephrotoxic agents may increase this risk. Additionally, the oral formulations of both medications have been associated with gastrointestinal irritation although data suggest concomitant use introduces little additional risk for adverse effects for most patients. [29558] [31826]
Ibritumomab Tiuxetan: (Major) During and after therapy, avoid the concomitant use of Yttrium (Y)-90 ibrutumomab tiuxetan with drugs that interfere with platelet function such as nonsteroidal antiinflammatory drugs (NSAIDs); the risk of bleeding may be increased. If coadministration with NSAIDs is necessary, monitor platelet counts more frequently for evidence of thrombocytopenia. [41826] (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Ibuprofen lysine: (Major) Because ibuprofen lysine exerts similar pharmacologic characteristics to other systemic NSAIDs, including COX-2 inhibitors, additive pharmacodynamic effects, including a potential increase for additive adverse GI effects, may be seen if ibuprofen lysine is used with other NSAIDs. In general, concurrent use of ibuprofen lysine and another NSAID should be avoided. [30115] [30569]
Iloprost: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Immune Globulin IV, IVIG, IGIV: (Moderate) Immune Globulin (IG) products have been reported to be associated with renal dysfunction, acute renal failure, osmotic nephrosis, and death. Patients predisposed to acute renal failure include patients receiving known nephrotoxic drugs like nonsteroidal anti-inflammatory drugs (NSAIDs) and salicylates. Coadminister IG products at the minimum concentration available and the minimum rate of infusion practicable. Also, closely monitor renal function. [6859] [7020] [7823]
Indapamide: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the natriuretic effect of diuretics in some patients. NSAIDS have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. Patients taking diuretics and NSAIDS concurrently are at higher risk of developing renal insufficiency. If an NSAID and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. [24233] [30489] [48492]
Indomethacin: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [35893] [45886]
Inotersen: (Moderate) Use caution with concomitant use of inotersen and nonsteroidal antiinflammatory drugs (NSAIDs) due to the risk of glomerulonephritis and nephrotoxicity as well as the potential risk of bleeding from thrombocytopenia. Consider discontinuation of NSAIDs in a patient taking inotersen with a platelet count of less than 50,000 per microliter. [63624]
Iodine; Potassium Iodide, KI: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Iodixanol: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Iohexol: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Iomeprol: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Ionic Contrast Media: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692]
Iopamidol: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Iopromide: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Ioversol: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Irbesartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Irbesartan; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Isosulfan Blue: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Isradipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Ivacaftor: (Minor) Increased monitoring is recommended if ivacaftor is administered concurrently with CYP2C9 substrates, such as ibuprofen. In vitro studies showed ivacaftor to be a weak inhibitor of CYP2C9. Co-administration may lead to increased exposure to CYP2C9 substrates; however, the clinical impact of this has not yet been determined. [48524]
Ketoprofen: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30548] [35893]
Ketorolac: (Contraindicated) Concomitant use of ketorolac with another NSAID is contraindicated. Increased adverse gastrointestinal effects are possible if ketorolac is used with other systemic nonsteroidal antiinflammatory drugs (NSAIDs). [28331] [30569] [35893]
Labetalol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
lamiVUDine; Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268]
Landiolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Leflunomide: (Moderate) In vitro studies indicate that the M1 metabolite of leflunomide inhibits cytochrome P450 2C9, the enzyme responsible for the metabolism of many NSAIDs. Leflunomide altered protein binding and thus, increased the free fraction of ibuprofen by 13% to 50%. The clinical significance of the interactions with NSAIDs is unknown. There was extensive concomitant use of NSAIDs in phase III clinical studies of leflunomide in the treatment of rheumatoid arthritis, and no clinical differential effects were observed. However, because some NSAIDs have been reported to cause hepatotoxic effects, some caution may be warranted in their use with leflunomide. [49634]
Levamlodipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Levobunolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
levoFLOXacin: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
Levomefolate: (Minor) L-methylfolate should be used cautiously in patients taking high doses of ibuprofen. Plasma concentrations of L-methylfolate may be reduced when used concomitantly with high doses of ibuprofen. Monitor patients for decreased efficacy of L-methylfolate if these agents are used together. [35581]
Levomilnacipran: (Moderate) Platelet aggregation may be impaired by SNRIs such as levomilnacipran due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Monitor for signs and symptoms of bleeding in patients taking levomilnacipran and NSAIDs. [55469]
Lisinopril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Lisinopril; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Lithium: (Moderate) Monitor serum lithium concentrations during concomitant nonsteroidal anti-inflammatory (NSAID) use; reduce the lithium dose based on serum lithium concentrations and clinical response. NSAIDs decrease renal blood flow, resulting in decreased renal clearance and increased serum lithium concentrations. [54241]
Lomustine, CCNU: (Major) Due to the bone marrow suppressive and thrombocytopenic effects of lomustine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, ASA, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [7668]
Losartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Losartan; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Lumacaftor; Ivacaftor: (Minor) Increased monitoring is recommended if ivacaftor is administered concurrently with CYP2C9 substrates, such as ibuprofen. In vitro studies showed ivacaftor to be a weak inhibitor of CYP2C9. Co-administration may lead to increased exposure to CYP2C9 substrates; however, the clinical impact of this has not yet been determined. [48524] (Minor) Lumacaftor; ivacaftor may alter the systemic exposure of ibuprofen. If used together, a dose adjustment of ibuprofen may be required to obtain the desired therapeutic effect and/or avoid adverse effects. Do not exceed the recommended maximum dose. Ibuprofen is a CYP2C9 substrate, and in vitro studies suggest that lumacaftor; ivacaftor has the potential to induce or inhibit CYP2C9. [34453] [34454] [34462] [59891]
Lumacaftor; Ivacaftor: (Minor) Lumacaftor; ivacaftor may alter the systemic exposure of ibuprofen. If used together, a dose adjustment of ibuprofen may be required to obtain the desired therapeutic effect and/or avoid adverse effects. Do not exceed the recommended maximum dose. Ibuprofen is a CYP2C9 substrate, and in vitro studies suggest that lumacaftor; ivacaftor has the potential to induce or inhibit CYP2C9. [34453] [34454] [34462] [59891]
Macimorelin: (Major) Avoid use of macimorelin with drugs that directly affect pituitary growth hormone secretion, such as nonsteroidal antiinflammatory drugs (NSAIDs). Healthcare providers are advised to discontinue NSAID therapy and observe a sufficient washout period before administering macimorelin. Use of these medications together may impact the accuracy of the macimorelin growth hormone test. [62723]
Magnesium Salicylate: (Major) Avoid concomitant use of ibuprofen with magnesium salicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Magnesium Sulfate; Potassium Sulfate; Sodium Sulfate: (Moderate) Use caution when prescribing sulfate salt bowel preparation in patients taking concomitant medications that may affect renal function such as nonsteroidal anti-inflammatory drugs (NSAIDs). [41573]
Mannitol: (Major) Avoid use of mannitol and nonsteroidal anti-inflammatory drugs (NSAIDs), if possible. If use together is necessary, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. Concomitant administration of nephrotoxic drugs, such as NSAIDs, increases the risk of renal failure after administration of mannitol. NSAIDs may reduce the natriuretic effect of diuretics in some patients. NSAIDS have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. [30489] [33007] [48492]
Mecamylamine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Meclofenamate Sodium: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30574] [35893]
Mefenamic Acid: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30570] [35893]
Meloxicam: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [29611] [35893]
Meloxicam; Rizatriptan: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [29611] [35893]
Mesalamine, 5-ASA: (Minor) The concurrent use of mesalamine with known nephrotoxic agents such as nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk of nephrotoxicity. [11423]
Methenamine; Sodium Salicylate: (Major) Avoid concomitant use of ibuprofen with sodium salicylate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Methotrexate: (Major) Do not administer nonsteroidal anti-inflammatory drugs (NSAIDs) before or concomitantly with high doses of methotrexate, such as used in the treatment of osteosarcoma. Concomitant administration of some NSAIDs with high dose methotrexate therapy has been reported to elevate and prolong serum methotrexate concentrations, resulting in deaths from severe hematologic and gastrointestinal toxicity. Use caution when NSAIDs are administered concomitantly with lower doses of methotrexate as they have been reported to reduce the tubular secretion of methotrexate in an animal model and may enhance its toxicity. Despite potential interactions, patients with rheumatoid arthritis (RA) are often receiving concurrent treatment with NSAIDs without apparent problems. However, these doses are lower than those used in psoriasis or malignancy; higher methotrexate doses may lead to unexpected toxicity in combination with NSAIDs. NSAIDs may be continued in patients with RA receiving treatment with methotrexate, although the possibility of increased toxicity has not been fully explored. [56263] [57771] [60517] [61900] [66594]
Methoxsalen: (Major) Preclinical data suggest agents that inhibit prostaglandin synthesis such as ibuprofen could decrease the efficacy of photosensitizing agents used in photodynamic therapy. Avoidance of ibuprofen before and during photodynamic therapy may be advisable. [29878]
Methyldopa: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
methylPREDNISolone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
metOLazone: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Metoprolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Metoprolol; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
miFEPRIStone: (Moderate) Mifepristone significantly increased exposure of drugs metabolized by CYP2C8/2C9 in interaction studies. Therefore, when mifepristone is used chronically, as in the treatment of Cushing's syndrome, use caution with coadministered CYP2C8/2C9 substrates, including the NSAIDs. Use the lowest doses of the substrate and patients should be monitored closely for adverse reactions. [48697]
Milnacipran: (Moderate) Platelet aggregation may be impaired by milnacipran due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Monitor for signs and symptoms of bleeding in patients taking milnacipran and NSAIDs. [28275] [29934]
mitoXANTRONE: (Major) Due to the thrombocytopenic effects of mitoxantrone, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [41139]
Moexipril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Mometasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Moxifloxacin: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
Nabumetone: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [31941] [35893]
Nadolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Naproxen: (Major) Avoid concomitant use of ibuprofen with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [32122] [35893]
Naproxen; Esomeprazole: (Major) Avoid concomitant use of ibuprofen with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [32122] [35893]
Naproxen; Pseudoephedrine: (Major) Avoid concomitant use of ibuprofen with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [32122] [35893]
Nebivolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Nelarabine: (Major) Due to the thrombocytopenic effects of nelarabine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [8493]
Neomycin: (Minor) It is possible that additive nephrotoxicity may occur in patients who receive NSAIDs concurrently with other nephrotoxic agents, such as aminoglycosides. [5046] [5062]
Neostigmine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Neostigmine; Glycopyrrolate: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
NiCARdipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
NIFEdipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
niMODipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Nisoldipine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Non-Ionic Contrast Media: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when given to patients receiving a contrast agents. When possible, withhold NSAID therapy during administration of a contrast agent. [28692] [28702]
Ofloxacin: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
OLANZapine; FLUoxetine: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Olmesartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Olmesartan; amLODIPine; hydroCHLOROthiazide, HCTZ: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Olmesartan; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Olopatadine; Mometasone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Omacetaxine: (Major) Avoid the concomitant use of omacetaxine and nonsteroidal antiinflammatory drugs (NSAIDs) when the platelet count is less than 50,000 cells/microliter due to an increased risk of bleeding. [52213]
Oritavancin: (Moderate) Ibuprofen is metabolized by CYP2C9; oritavancin is a weak CYP2C9 inhibitor. Coadministration may result in elevated ibuprofen plasma concentrations. If these drugs are administered concurrently, monitor patients for NSAID-induced toxicity, such as nausea, GI bleeding, or renal dysfunction. [11310] [11311] [11319] [57741]
Oxaprozin: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30565] [35893]
PACLitaxel: (Major) Due to the thrombocytopenic effects of paclitaxel, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5938]
Pamidronate: (Moderate) Monitor renal function during concomitant pamidronate and nonsteroidal antiinflammatory drug use due to risk for additive nephrotoxicity. [31027] [32122]
PARoxetine: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
PEMEtrexed: (Major) Avoid administration of ibuprofen for 2 days before, the day of, and 2 days after administration of pemetrexed in patients with a creatinine clearance (CrCl) between 45 mL/min and 79 mL/min due to the risk of increased pemetrexed exposure resulting in an increase in pemetrexed-related adverse reactions. If concomitant use is unavoidable, monitor these patients more frequently for myelosuppression, nephrotoxicity, and gastrointestinal toxicity. Pemetrexed is an OAT3 substrate and ibuprofen is an OAT3 inhibitor. Coadministration with ibuprofen 400 mg four times daily increased pemetrexed exposure by approximately 20% in patients with normal renal function (CrCl greater than 80 mL/min). In vitro data predict that other NSAIDS (e.g., naproxen, diclofenac, and celecoxib) would not increase pemetrexed exposure to a clinically significant extent. [28376] [67147]
Pentamidine: (Major) Avoid concurrent or sequential use of pentamidine with ibuprofen. Coadministration may increase the risk for drug-induced nephrotoxicity. Closely monitor renal function if coadministration is unavoidable. [28879]
Pentosan: (Moderate) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Pentostatin: (Major) Due to the thrombocytopenic effects of pentostatin, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [5512]
Perindopril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Perindopril; amLODIPine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Pexidartinib: (Moderate) Monitor for evidence of hepatotoxicity if pexidartinib is coadministered with ibuprofen. Avoid concurrent use in patients with increased serum transaminases, total bilirubin, or direct bilirubin (more than ULN) or active liver or biliary tract disease. [63549] [64535]
Phenoxybenzamine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Phentolamine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Photosensitizing agents (topical): (Moderate) Agents that inhibit prostaglandin synthesis such as nonsteroidal antiinflammatory drugs (NSAIDs), could decrease the efficacy of photosensitizing agents used in photodynamic therapy. Avoidance of NSAIDs before and during photodynamic therapy may be advisable. [42968]
PHYSostigmine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Pindolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Pioglitazone; Glimepiride: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
Piroxicam: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [29613] [35893]
Platelet Inhibitors: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Pneumococcal Vaccine, Polyvalent: (Moderate) Concomitant administration of antipyretics, such as nonsteroidal antiinflammatory drugs (NSAIDS), may decrease an individual's immunological response to the pneumococcal vaccine. A post-marketing study conducted in Poland using a non-US vaccination schedule (2, 3, 4, and 12 months of age) evaluated the impact of prophylactic oral acetaminophen on antibody responses to Prevnar 13. Data show that acetaminophen, given at the time of vaccination and then dosed at 6 to 8 hour intervals for 3 doses on a scheduled basis, reduced the antibody response to some serotypes after the third dose of Prevnar 13 when compared to the antibody responses of infants who only received antipyretics 'as needed' for treatment. However, reduced antibody responses were not observed after the fourth dose of Prevnar 13 with prophylactic acetaminophen. [39165]
Polyethylene Glycol; Electrolytes: (Moderate) Use caution when prescribing sulfate salt bowel preparation in patients taking concomitant medications that may affect renal function such as nonsteroidal anti-inflammatory drugs (NSAIDs). [41573]
Polyethylene Glycol; Electrolytes; Ascorbic Acid: (Moderate) Use caution when prescribing sulfate salt bowel preparation in patients taking concomitant medications that may affect renal function such as nonsteroidal anti-inflammatory drugs (NSAIDs). [41573]
Polymyxin B: (Major) The chronic coadministration of systemic polymyxins may increase the risk of developing nephrotoxicity, even in patients who have normal renal function. Nonsteroidal antiinflammatory drugs (NSAIDs) may increase the risk for nephrotoxicity when used concurrently. Monitor patients for changes in renal function if these drugs are coadministered. Since Polymyxin B is eliminated by the kidney, coadministration with other potentially nephrotoxic drugs, including nonsteroidal antiinflammatory drugs (NSAIDs), may theoretically increase serum concentrations of either drug. [28447]
Potassium Acetate: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium Bicarbonate: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium Chloride: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium Citrate: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium Citrate; Citric Acid: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium Gluconate: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium Iodide, KI: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Potassium: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
PRALAtrexate: (Major) Renal elimination accounts for approximately 34% of the overall clearance of pralatrexate. Concomitant administration of drugs that undergo substantial renal clearance, such as nonsteroidal antiinflammatory drugs (NSAIDs), may result in delayed clearance of pralatrexate. [36890]
Prasugrel: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Prazosin: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
prednisoLONE: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
predniSONE: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Pretomanid: (Major) Avoid coadministration of pretomanid with ibuprofen, especially in patients with impaired hepatic function, due to increased risk for hepatotoxicity. Monitor for evidence of hepatotoxicity if coadministration is necessary. If new or worsening hepatic dysfunction occurs, discontinue hepatotoxic medications. [63549] [64561]
Probenecid: (Major) Probenecid can decrease the renal clearance of nonsteroidal antiinflammatory agents (NSAIDs). Reduction of the NSAID dose may be necessary when it is used together with probenecid. [5071]
Probenecid; Colchicine: (Major) Probenecid can decrease the renal clearance of nonsteroidal antiinflammatory agents (NSAIDs). Reduction of the NSAID dose may be necessary when it is used together with probenecid. [5071]
Procarbazine: (Major) Due to the thrombocytopenic effects of procarbazine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [5356]
Propranolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
pyRIDostigmine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Quinapril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Quinapril; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Quinolones: (Moderate) Use quinolones and nonsteroidal anti-inflammatory drugs (NSAIDs) concomitantly with caution due to potential increased risk of CNS stimulation and convulsive seizures. NSAIDs in combination with very high doses of quinolones have been shown to provoke convulsions in preclinical studies and postmarketing. [28423] [28424] [28764] [29947] [43411] [65562]
Ramipril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Reteplase, r-PA: (Moderate) NSAIDs can cause GI bleeding, inhibit platelet aggregation, prolong bleeding time; these pharmacodynamic effects may be increased when administered to patients receiving thrombolytic agents. Patients receiving these drugs concurrently should be monitored closely for bleeding. [28469] [30569]
Riluzole: (Moderate) Monitor for signs and symptoms of hepatic injury during coadministration of riluzole and ibuprofen. Concomitant use may increase the risk for hepatotoxicity. Discontinue riluzole if clinical signs of liver dysfunction are present. [29747] [44120] [44121] [63549]
Risedronate: (Minor) Monitor for gastrointestinal adverse events during concurrent use of risedronate and nonsteroidal antiinflammatory drugs. Both medications have been associated with gastrointestinal irritation although data suggest concomitant use introduces little additional risk for adverse effects for most patients. [42080]
Rivaroxaban: (Major) An additive risk of bleeding may be seen in patients receiving anticoagulants in combination with other agents known to increase the risk of bleeding such as nonsteroidal antiinflammatory drugs (NSAIDs). Monitor clinical and laboratory response closely during concurrent use. [29732] [40621] [49946]
Rivastigmine: (Moderate) NSAIDs may cause additive pharmacodynamic GI effects with cholinesterase inhibitors, leading to gastrointestinal intolerance. Patients receiving concurrent NSAIDs should be monitored closely for symptoms of active or occult gastrointestinal bleeding. While NSAIDs appear to suppress microglial activity, which in turn may slow inflammatory neurodegenerative processes important for the progression of Alzheimer's disease (AD), there are no clinical data at this time to suggest that NSAIDs alone or as combined therapy with AD agents result in synergistic effects in AD. [27344]
Sacubitril; Valsartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Salsalate: (Major) Avoid concomitant use of ibuprofen with salsalate due to an increased risk of gastrointestinal toxicity and renal impairment, with little or no increase in efficacy. [35893] [61171]
Selective serotonin reuptake inhibitors: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Sertraline: (Moderate) Monitor for signs and symptoms of bleeding during concomitant selective serotonin reuptake inhibitor (SSRI) and nonsteroidal antiinflammatory drug (NSAID) use due to increased risk for bleeding. Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. [27414] [32127]
Sodium Phosphate Monobasic Monohydrate; Sodium Phosphate Dibasic Anhydrous: (Moderate) Concomitant use of medicines with potential to alter renal perfusion or function such as nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk of acute phosphate nephropathy in patients taking sodium phosphate monobasic monohydrate; sodium phosphate dibasic anhydrous. [32159] [32160]
Sodium picosulfate; Magnesium oxide; Anhydrous citric acid: (Moderate) Use caution when prescribing sodium picosulfate; magnesium oxide; anhydrous citric acid in patients taking concomitant medications that may affect renal function such as nonsteroidal anti-inflammatory drugs (NSAIDs). [51258]
Sodium Sulfate; Magnesium Sulfate; Potassium Chloride: (Moderate) Monitor serum potassium concentrations closely if potassium supplements and nonsteroidal anti-inflammatory drugs (NSAIDs) are used together. Concomitant use may increase the risk of hyperkalemia. [30272] [53793]
Sotalol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Sparsentan: (Moderate) Monitor for worsening renal function during concomitant use of sparsentan and nonsteroidal antiinflammatory drugs (NSAIDs), including selective cyclooxygenase (COX-2) inhibitors. Concomitant use increases the risk for nephrotoxicity, especially in patients with additional risk factors such as hypovolemia and chronic renal impairment. [68641]
Spironolactone: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant spironolactone and nonsteroidal antiinflammatory drug (NSAID) use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [32018] [48492]
Spironolactone; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant spironolactone and nonsteroidal antiinflammatory drug (NSAID) use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [32018] [48492]
Streptomycin: (Moderate) It is possible that additive nephrotoxicity may occur in patients who receive nonsteroidal anti-inflammatory drugs (NSAIDs) concurrently with other nephrotoxic agents, such as streptomycin. [28370] [30110] [30268]
Sulfonylureas: (Moderate) NSAIDs may enhance hypoglycemia in diabetic patients via inhibition of prostaglandin synthesis, which indirectly increases insulin secretion. If NSAIDs are administered or discontinued in patients receiving oral antidiabetic agents, patients should be monitored for hypoglycemia or loss of blood glucose control. No clinically significant interaction between sulindac at daily doses of 400 mg and oral hypoglycemic agents has been observed. Sulindac, its sulfide metabolite, and sulfonylureas are highly bound to protein. Sulindac could displace the sulfonylureas, altering hypoglycemic activity. Careful patient monitoring is recommended to ensure that no change in their diabetes medicine dosage is required. A sulfonylurea dose adjustment may be needed, especially if sulindac doses greater than 400 mg daily are used or if the drug combination is used in patients with renal impairment or other metabolic defects that might increase sulindac blood concentrations. [24711] [29374] [51000]
Sulindac: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [28340] [35893]
Sulopenem Etzadroxil; Probenecid: (Major) Probenecid can decrease the renal clearance of nonsteroidal antiinflammatory agents (NSAIDs). Reduction of the NSAID dose may be necessary when it is used together with probenecid. [5071]
SUMAtriptan; Naproxen: (Major) Avoid concomitant use of ibuprofen with any other NSAID due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [32122] [35893]
Tacrolimus: (Moderate) Monitor patients for signs of worsening renal function during coadministration of tacrolimus and nonsteroidal antiinflammatory drugs. Coadministration may increase the risk for drug-induced nephrotoxicity. [28611]
Telavancin: (Minor) Concurrent or sequential use of telavancin with drugs that inhibit renal prostaglandins such as nonsteroidal antiinflammatory drugs (NSAIDS) may lead to additive nephrotoxicity. Closely monitor renal function and adjust telavancin doses based on calculated creatinine clearance. [36615] [7020]
Telmisartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Telmisartan; amLODIPine: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Telmisartan; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Temozolomide: (Major) Myelosuppression, primarily neutropenia and thrombocytopenia, is the dose-limiting toxicity of temozolomide. Due to the thrombocytopenic effects of temozolomide, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, ASA, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [7578]
Tenecteplase: (Moderate) NSAIDs can cause GI bleeding, inhibit platelet aggregation, prolong bleeding time; these pharmacodynamic effects may be increased when administered to patients receiving thrombolytic agents. Patients receiving these drugs concurrently should be monitored closely for bleeding. [28469] [30569]
Tenofovir Alafenamide: (Moderate) Concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs) and tenofovir alafenamide may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [61413] [71829] [72477]
Tenofovir Disoproxil Fumarate: (Moderate) Avoid administering tenofovir, PMPA concurrently with or recently after a nephrotoxic agent, such as high-dose or multiple nonsteroidal antiinflammatory drugs (NSAIDs). Cases of acute renal failure, some requiring hospitalization and renal replacement therapy, have been reported after high-dose or multiple NSAIDs were initiated in patients who appeared stable on tenofovir. Consider alternatives to NSAIDs in patients at risk for renal dysfunction. If these drugs must be coadministered, carefully monitor the estimated creatinine creatinine, serum phosphorus, urine glucose, and urine protein prior to, and periodically during, treatment. [28193] [30268]
Terazosin: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Tezacaftor; Ivacaftor: (Minor) Increased monitoring is recommended if ivacaftor is administered concurrently with CYP2C9 substrates, such as ibuprofen. In vitro studies showed ivacaftor to be a weak inhibitor of CYP2C9. Co-administration may lead to increased exposure to CYP2C9 substrates; however, the clinical impact of this has not yet been determined. [48524]
Thiazide diuretics: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Thioguanine, 6-TG: (Major) Due to the thrombocytopenic effects of thioguanine, an additive risk of bleeding may be seen in patients receiving concomitant anticoagulants, NSAIDs, platelet inhibitors, including aspirin, strontium-89 chloride, and thrombolytic agents. In addition, large doses of salicylates (>= 3-4 g/day) can cause hypoprothrombinemia, an additional risk factor for bleeding. [5170] [5853]
Thrombolytic Agents: (Moderate) NSAIDs can cause GI bleeding, inhibit platelet aggregation, prolong bleeding time; these pharmacodynamic effects may be increased when administered to patients receiving thrombolytic agents. Patients receiving these drugs concurrently should be monitored closely for bleeding. [28469] [30569]
Ticagrelor: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Timolol: (Moderate) Monitor blood pressure during concomitant beta-blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of beta-blockers may be diminished by NSAIDs. [32122]
Tirofiban: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Tobacco: (Major) Advise patients to avoid smoking tobacco while taking nonsteroidal anti-inflammatory drugs (NSAIDs). Concomitant use of NSAIDs with tobacco smoking may enhance the risk of gastrointestinal side effects, including peptic ulcer and GI bleeding. Patients using tobacco and NSAIDs concurrently should be monitored closely for GI adverse reactions. [28327] [30496] [32018] [56268]
Tobramycin: (Moderate) It is possible that additive nephrotoxicity may occur in patients who receive nonsteroidal anti-inflammatory drugs (NSAIDs) concurrently with other nephrotoxic agents, such as tobramycin. [28370] [30110] [30268]
Tolmetin: (Major) Avoid concomitant use of ibuprofen with any other NSAID, including COX-2 inhibitors, due to the risk of additive serious NSAID toxicities including but not limited to GI bleeding, GI perforation, or peptic ulcers. [30242] [35893]
Torsemide: (Moderate) If a nonsteroidal anti-inflammatory drug (NSAID) and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. Patients taking diuretics and NSAIDs concurrently are at higher risk of developing renal insufficiency. NSAIDs may reduce the natriuretic effect of diuretics in some patients. NSAIDs have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. [30489] [48492]
Trandolapril: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
Trandolapril; Verapamil: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489] (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin-converting enzyme (ACE) inhibitor and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of ACE inhibitors may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of ACE inhibitors and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [32122] [61325]
traZODone: (Moderate) Platelet aggregation may be impaired by trazodone due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Patients should be instructed to monitor for signs and symptoms of bleeding while taking trazodone concurrently with medications that impair platelet function and to promptly report any bleeding events to the practitioner. [38831]
Treprostinil: (Moderate) NSAIDs may decrease the effect of antihypertensive agents through various mechanisms, including renal and peripheral vasoactive pathways. [4087]
Triamcinolone: (Moderate) Monitor for gastrointestinal toxicity during concurrent corticosteroid and nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of GI bleeding. [24574] [29611] [35893]
Triamterene: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant triamterene and ibuprofen use. Nonsteroidal antiinflammatory drugs (NSAIDs) may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Triamterene; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant triamterene and ibuprofen use. Nonsteroidal antiinflammatory drugs (NSAIDs) may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Urea: (Moderate) Nonsteroidal anti-inflammatory drugs (NSAIDs) may reduce the natriuretic effect of diuretics in some patients. NSAIDS have been associated with an inhibition of prostaglandin synthesis, which may result in reduced renal blood flow leading to renal insufficiency and increases in blood pressure that are often accompanied by peripheral edema and weight gain. Patients taking diuretics and NSAIDS concurrently are at higher risk of developing renal insufficiency. If an NSAID and a diuretic are used concurrently, carefully monitor the patient for signs and symptoms of decreased renal function and diuretic efficacy. [30489] [48492]
valACYclovir: (Moderate) Monitor patients for signs of worsening renal function during coadministration of valacyclovir and nonsteroidal antiinflammatory drugs. Coadministration may increase the risk for drug-induced nephrotoxicity. [29970] [56268]
valGANciclovir: (Minor) Concurrent use of nephrotoxic agents, such as NSAIDs, with valganciclovir should be done cautiously to avoid additive nephrotoxicity. [5193]
Valsartan: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860]
Valsartan; hydroCHLOROthiazide, HCTZ: (Moderate) Monitor blood pressure and renal function periodically during concomitant angiotensin II blocker and nonsteroidal anti-inflammatory drug (NSAID) use. The antihypertensive effect of angiotensin II blockers may be diminished by NSAIDs. In persons who are elderly, volume-depleted, or with compromised renal function, coadministration of angiotensin II blockers and NSAIDs may result in deterioration of renal function, including possible acute renal failure; these effects are usually reversible. [27388] [27991] [28608] [29130] [32122] [60860] (Moderate) Monitor blood pressure as well as for signs of worsening renal function and loss of diuretic efficacy, including antihypertensive effects, during concomitant nonsteroidal antiinflammatory drug (NSAID) and thiazide diuretic use. NSAIDs may cause a dose-dependent reduction in renal blood flow, which may precipitate overt renal decompensation, and concomitant diuretic use increases the risk of this reaction. NSAIDs have been shown to reduce the natriuretic effect of thiazide diuretics and are associated with fluid retention which may blunt the cardiovascular effects of diuretics. [35893] [48492]
Vancomycin: (Minor) It is possible that additive nephrotoxicity may occur in patients who receive NSAIDs concurrently with other nephrotoxic agents, including vancomycin. [28370] [28468] [30110] [30268]
Vemurafenib: (Major) Concomitant use of vemurafenib and ibuprofen may result in increased ibuprofen concentrations. Vemurafenib is a CYP2C9 inhibitor and ibuprofen is a CYP2C9 substrate. Patients should be monitored for toxicity. [34454] [45335]
Venlafaxine: (Moderate) Platelet aggregation may be impaired by venlafaxine due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Monitor patients for signs and symptoms of bleeding when coadministering venlafaxine with NSAIDs. [28275]
Verapamil: (Moderate) If nonsteroidal anti-inflammatory drugs (NSAIDs) and an antihypertensive drug are concurrently used, carefully monitor the patient for signs and symptoms of renal insufficiency and blood pressure control. Doses of antihypertensive medications may require adjustment in patients receiving concurrent NSAIDs. NSAIDs, to varying degrees, have been associated with an elevation in blood pressure. This effect is most significant in patients receiving concurrent antihypertensive agents and long-term NSAID therapy. NSAIDs cause a dose-dependent reduction in prostaglandin formation, which may result in a reduction in renal blood flow leading to renal insufficiency and an increase in blood pressure that are often accompanied by peripheral edema and weight gain. Patients who rely upon renal prostaglandins to maintain renal perfusion may have acute renal blood flow reduction with NSAID usage. Elderly patients may be at increased risk of adverse effects from combined long-term NSAID therapy and antihypertensive agents, especially diuretics, due to age-related decreases in renal function and an increased risk of stroke and coronary artery disease. [24233] [26486] [27388] [30489]
Verteporfin: (Moderate) Use caution if coadministration of verteporfin with nonsteroidal anti-inflammatory drugs is necessary due to the risk of decreased verteporfin efficacy. Oxaprozin may additionally worsen photosensitivity. Verteporfin is a light-activated drug. Once activated, local damage to neovascular endothelium results in a release of procoagulant and vasoactive factors resulting in platelet aggregation, fibrin clot formation, and vasoconstriction. Concomitant use of drugs that decrease platelet aggregation like nonsteroidal anti-inflammatory drugs could decrease the efficacy of verteporfin therapy. [30003]
Vilazodone: (Moderate) Platelet aggregation may be impaired by vilazodone due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Patients should be instructed to monitor for signs and symptoms of bleeding while taking vilazodone concurrently with NSAIDs and to promptly report any bleeding events to the practitioner. [43177]
Voclosporin: (Moderate) Concomitant use of voclosporin and nonsteroidal anti-inflammatory drugs (NSAIDs) may result in additive nephrotoxicity. Monitor for renal toxicity if concomitant use is required. [66336] [66357]
Vorapaxar: (Moderate) Monitor for signs and symptoms of bleeding during concomitant platelet inhibitor and chronic nonsteroidal antiinflammatory drug (NSAID) use. Concomitant use increases the risk of bleeding. [28435] [36055]
Voriconazole: (Moderate) Voriconazole is a substrate and inhibitor of cytochrome P450 isoenzyme 2C9, which is the isoenzyme responsible for the metabolism of ibuprofen. Thus, increased plasma concentrations of ibuprofen is possible. The clinical significance of this potential interaction is unknown. If voriconazole is administered concurrently with ibuprofen, monitor for NSAID-related side-effects, such as fluid retention or GI irritation, and adjust the dose of the NSAID, if needed. [34447] [4882]
Vortioxetine: (Moderate) Platelet aggregation may be impaired by vortioxetine due to platelet serotonin depletion, possibly increasing the risk of a bleeding complication (e.g., gastrointestinal bleeding, ecchymoses, epistaxis, hematomas, petechiae, hemorrhage) in patients receiving nonsteroidal antiinflammatory drugs (NSAIDs). Bleeding events related to drugs that inhibit serotonin reuptake have ranged from ecchymosis to life-threatening hemorrhages. Patients should be instructed to monitor for signs and symptoms of bleeding while taking vortioxetine concurrently with medications which impair platelet function and to promptly report any bleeding events to the practitioner. [56041]
Warfarin: (Moderate) Monitor patients for signs or symptoms of bleeding during concurrent use of warfarin and nonsteroidal antiinflammatory drugs (NSAIDs). To minimize the potential for GI bleeding, use the lowest effective NSAID dose for the shortest possible duration. If signs or symptoms of bleeding occur, promptly evaluate and treat. Systemic hematological effects may also occur with the use of topical NSAIDs. NSAIDs inhibit platelet aggregation and may prolong bleeding time in some patients. [28549] [33554] [56268] [61088]
Zafirlukast: (Minor) Zafirlukast inhibits the CYP2C9 isoenzymes and should be used cautiously should be used cautiously in patients stabilized on drugs metabolized by CYP2C9, such as ibuprofen. [4718] [4948]
Zoledronic Acid: (Moderate) Monitor renal function during concomitant zoledronic acid and nonsteroidal antiinflammatory drug use due to risk for additive nephrotoxicity. [32122] [58724]
Monitoring Parameters
blood pressure
CBC
LFTs
serum creatinine/BUN
US Drug Names
Advil
Advil Children's
Advil Children's Fever
Advil Infants'
Advil Junior Strength
Advil Migraine
ALIVIO
Caldolor
Children's Ibuprofen
ElixSure IB
Genpril
Ibren
IBU
Ibupak
Midol
Midol Cramps and Body Aches
Motrin
Motrin Children's
Motrin IB
Motrin Infants'
Motrin Junior Strength
Motrin Migraine Pain
PediaCare Children's Pain Reliever/Fever Reducer IB
PediaCare Infants' Pain Reliever/Fever Reducer IB
Samson-8
Toxicology Saliva Collection
References
805 - The sixth report of the Joint National Committee on detection, evaluation, and treatment of high blood pressure. National Institute of Health publication No 99-4080. 1997;1-64.
4087 - Frishman WH. Effects of nonsteroidal anti-inflammatory drug therapy on blood pressure and peripheral edema. Am J Cardiol 2002;89(suppl):18D-25D.
4716 - Yasmin (ethinyl estradiol-drosperinone) package insert. Montville, NJ: Berlex Laboratories; 2003 Jun.
4718 - Hansten PD, Horn JR. Cytochrome P450 Enzymes and Drug Interactions, Table of Cytochrome P450 Substrates, Inhibitors, Inducers and P-glycoprotein, with Footnotes. In: The Top 100 Drug Interactions - A guide to Patient Management. 2008 Edition. Freeland, WA: H&H Publications; 2008:142-157.
4736 - Myleran (busulfan) package insert. Research Triangle Park, NC: GlaxoSmithKline; 2004 Jan.
4757 - Leukeran (chlorambucil) package insert. Research Triangle Park, NC: GlaxoSmithKline; 2011 Oct.
4882 - VFEND (voriconazole) tablets, suspension, and injection package insert. New York, NY: Pfizer Inc; 2025 Mar.
4948 - Accolate (zafirlukast) package insert. Wilmington, DE: AstraZeneca; 2015 Dec.
5046 - Celebrex (celecoxib) package insert. New York, NY: Pfizer, Inc.; 2013 Jan.
5062 - Amphocin (amphotericin B) package insert. Kalamazoo, MI: Pharmacia Corporation; 2003 Sep.
5071 - Brouwers JR, de Smet PA. Pharmacokinetic-pharmacodynamic drug interactions with nonsteroidal anti-inflammatory drugs. Clin Pharmacokinet 1994;27:462-85.
5170 - Hayes, AH. Therapeutic implications of drug interactions with acetaminophen and aspirin. Arch Intern Med 1981;141:301-4.
5193 - Valcyte (valganciclovir hydrochloride) package insert. South San Francisco, CA: Genentech USA, Inc.; 2021 Dec.
5235 - Docetaxel concentrate solutions for injection package insert. Bridgewater, NJ: Winthrop US; 2011 Apr.
5356 - Matulane (procarbazine) package insert. Gaithersburg, MD: sigma-tau Pharmaceuticals, Inc.; 2002 July.
5512 - Nipent® (pentostatin for injection) package insert. Lake Forest, IL: Hospira, Inc.; 2007 Apr.
5853 - Tabloid (thioguanine) package insert. Research Triangle Park, NC: GlaxoSmithKline; 2008 Oct.
5938 - Taxol (paclitaxel) package insert. Princeton, NJ: Bristol-Meyers Squibb; 2011 Apr.
5946 - BiCNU (carmustine) injection package insert. Edison, NJ: Heritage Pharmaceuticals Inc.; 2013 Apr.
6144 - Vioxx (rofecoxib) package insert. Whitehouse Station, NJ: Merck & amp; Co., Inc.; 2004 Mar.
6859 - Insel PA. Analgesic-antipyretic and antiinflammatory agents and drugs employed in the treatment of gout. In: Hardman JG, Limbird LE, Molinoff PB, et al., eds. Goodman and Gilman's the pharmacological basis of therapeutics, 9th edn. New York: McGraw Hill, 1996;617-657.
7020 - Perez Gutthann S, Garcia Rodriguez LA, Raiford DS, et al. Nonsteroidal anti-inflammatory drugs [NSAIDs] and the risk of hospitalization for acute renal failure. Arch Intern Med 1996;156(21):2433-9.
7226 - Cladribine injection package insert. Lake Zurich, IL: Fresenius Kabi USA, LLC; 2016 Aug.
7446 - Floxuridine Injection package insert. Bedford, OH: Bedford Laboratories; 2000 Feb.
7557 - Clolar (clofarabine) package insert. Cambridge, MA: Genzyme Corporation; 2010 Dec.
7578 - Temodar (temozolomide) package insert. Whitehouse Station, NJ: Schering Corporation; 2011 Feb.
7668 - CeeNU® (Lomustine) package insert. Princeton, NJ: Bristol Laboratories Oncology Products; 2003.
7823 - Doans extra strength (magnesium salicylate tetrahydrate) package insert. Sommerville, NJ: Ducere Pharma; 2016 Jun.
7945 - Cytosar-U® (cytarabine, ARA-C) package insert. Kalamazoo, MI: Pharmacia & Upjohn Company; 1999 Feb.
7996 - DTIC-Dome® (dacarbazine, DTIC) package insert. Bedford, OH: Ben Venue Laboratories; 1998.
8493 - Arranon (nelarabine) package insert. Research Triangle Park, NC: GlaxoSmithKline: October 2005.
10457 - DDAVP nasal spray (desmopressin acetate) package insert. Parsippany, NJ: Ferring Pharmaceuticals Inc.; 2018 Sept.
10458 - Garcia EB, Ruitenberg A, Madretsma GS, et al. Hyponatraemic coma induced by desmopressin and ibuprofen in a woman with von Willebrand's disease. Haemophilia 2003;9:232-4.
11310 - Hynninen V, Olkkola KT, Leino K, et al. Effects of the antifungals voriconazole and fluconazole on the pharmacokinetics of S-(+)- and R-(-)-ibuprofen. Antimicrob Agents Chemother 2006;50:1967-72.
11311 - Hamman MA, Thompson GA, Hall SD. Regioselective and stereoselective metabolism of ibuprofen by human cytochrome P450 2C. Biochem Pharmacol 1997;54;1:33-41.
11319 - Kirchheiner J, Meineke I, Freytag G, et al. Enantiospecific effects of cytochrome P450 2C9 amino acid variants on ibuprofen pharmacokinetics and on the inhibition of cyclooxygenases 1 and 2. Clin Pharmacol Ther 2002;72:62-75.
11423 - Lialda (mesalamine delayed-release tablets) package insert. Lexington, MA: Shire US, Inc.; 2023 Oct.
21333 - Lewis DW, Kellstein D, Dahl G, et al. Children's ibuprofen suspension for the acute treatment of pediatric migraine. Headache. 2002;42:780-6
24179 - Konstan MW, Byard PJ, Hoppel CL, et al. Effect of high-dose ibuprofen in patients with cystic fibrosis. N Engl J Med 1995;332:848-54.
24233 - The sixth report of the Joint National Committee on detection, evaluation, and treatment of high blood pressure. National Institute of Health publication No 99-4080. 1997;1-64.
24245 - Hamalainen ML, Hoppu K, Vlakeila E, et al. Ibuprofen or acetaminophen for the acute treatment of migraine in children: a double-blind, randomized, placebo-controlled, crossover study. Neurology 1997;48:103-7.
24574 - Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. Ann Intern Med 1991;115:787-96.
24711 - Kubacka RT, Antal EJ, Juhl RP et al. Effects of aspirin and ibuprofen on the pharmacokinetics and pharmacodynamics of glyburide in healthy subjects. Ann Pharmacother 1996;30:20-6.
25082 - Rosenblatt M, Mindel J. Spontaneous hyphema associated with ingestion of Ginkgo biloba extract. N Engl J Med 1997;336:1108.
25083 - Rowin J, Lewis SL. Spontaneous bilateral subdural hematomas associated with chronic Ginkgo biloba ingestion. Neurology 1996;46:1775-6.
25273 - Lamant V, Mauco G, Braquet P, et al. Inhibition of the metabolism of platelet activating factor (PAF-acether) by three specific antagonists from Ginkgo biloba. Bio Pharmacol 1987;36:2749-52.
25588 - Ariga T. Platelet aggregation inhibitor in garlic (letter). Lancet 1980;i:150.
26486 - Johnson AG. NSAIDs and increased blood pressure. What is the clinical significance? Drug Safety 1997;17:277-89.
27344 - Veld BA, Ruitenberg A, Hofman A, et al. Nonsteroidal antiinflammatory drugs and the risk of Alzheimer's disease. N Engl J Med 2001;345:1515-1521.
27388 - Frishman WH. Effects of nonsteroidal anti-inflammatory drug therapy on blood pressure and peripheral edema. Am J Cardiol 2002;89(suppl):18D-25D.
27414 - Dalton, SO, Johansen C, Mellemkjaer L, et al. Use of selective serotonin reuptake inhibitors and the risk of upper gastrointestinal tract bleeding: a population-based cohort study. Arch Intern Med 2003;163:59-64.
27615 - Mulato AS, Ho ES, Cihlar T. Nonsteroidal anti-inflammatory drugs efficiently reduce the transport and cytotoxicity of adefovir mediated by the human renal organic anion transporter 1. J Pharmacol Exper Ther 2000;295:10-15.
27710 - Ashwath ML, Katner HP. Recurrent aseptic meningitis due to different non-steroidal anti-inflammatory drugs including rofecoxib. Postgrad Med J 2003;79:295-6.
27990 - Inspra (eplerenone) package insert. Morgantown, WV: Viatris Specialty, LLC; 2025 Jun.
27991 - Atacand (candesartan) package insert. Baudette, MN: ANI Pharmaceuticals, Inc; 2020 Jun.
28024 - Carbatrol (carbamazepine extended-release capsules) package insert. Lexington, MA: Takeda Pharmaceuticals America, Inc.; 2023 Apr.
28193 - Viread (tenofovir disoproxil fumarate) package insert. Foster City, CA: Gilead Sciences, Inc; 2019 Apr.
28272 - Lanoxin (digoxin) tablets package insert. St. Michael, Barbados: Concordia Pharmaceuticals Inc.; 2020 Apr..
28275 - Effexor (venlafaxine) package insert. Philadelphia, PA: Wyeth Pharmaceuticals, Inc.; 2021 Sept.
28317 - Celebrex (celecoxib) package insert. New York, NY: Pfizer, Inc.; 2013 Jan.
28327 - Zevin S, Benowitz NL. Drug interactions with tobacco smoking: an update. Clin Pharmacokinet 1999;36:425-38.
28331 - Ketorolac tromethamine tablets package insert. Morgantown, WV: Mylan Pharmaceuticals, Inc.; 2024 Aug.
28333 - Amphocin (amphotericin B) package insert. Kalamazoo, MI: Pharmacia Corporation; 2003 Sep.
28340 - Clinoril (sulindac) package insert. Whitehouse Station, NJ: Merck Co., Inc.; 2007 Feb.
28370 - Dolobid® (diflunisal) package insert. West Point, PA: Merck; 1998 Jul.
28376 - Alimta (pemetrexed) injection package insert. Indianapolis, IN: Lilly USA, LLC; 2022 Aug.
28377 - Foscavir (foscarnet) package insert. Lake Forest, IL: Hospira, Inc.; 2020 Oct.
28388 - Cidofovir injection solution package insert. Morgantown, WV: Mylan Institutional LLC; 2021 Apr.
28423 - Avelox (moxifloxacin) package insert. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc.; 2025 July.
28424 - Factive (gemifloxacin mesylate) package insert. Toronto, ON: Merus Labs International, Inc.; 2019 May.
28435 - Plavix (clopidogrel) package insert. Morristown, NJ: Sanofi-Aventis U.S. LLC; 2025 May.
28447 - Polymyxin B package insert. Big Flats, NY: X-Gen Pharmaceuticals, Inc.; 2015 Dec.
28468 - Vancocin HCl capsules (vancomycin hydrochloride) package insert. Baudette, MN: Ani Pharmaceuticals, Inc.; 2021 Dec.
28469 - Abbokinase® (urokinase) package insert. North Chicago, IL: Abbott Laboratories, INC; 2002 Oct.
28470 - Vaes LP, Chyka PA. Interactions of warfarin with garlic, ginger, ginkgo, or ginseng: nature of the evidence. Review. Ann Pharmacother 2000;34:1478-82.
28549 - Warfarin tablets package insert. Parsippany, NJ: Teva Pharmaceuticals; 2025 Jun.
28608 - Cozaar (losartan potassium) package insert. Jersey City, NJ: Organon & Co., Inc.; 2025 Jun.
28611 - Prograf (tacrolimus) capsules, injection, and granules for oral suspension package insert. Northbrook, IL: Astellas Pharma US, Inc.; 2023 Aug.
28644 - Fosamax (alendronate) tablets and oral solution package insert. Jersey City, NJ: Organon LLC; 2021 Jun.
28646 - Marshall WF, Blair JE. The cephalosporins. Mayo Clinic Proc 1999;74:187-95.
28692 - Thomsen HS, Bush WH. Adverse effects of contrast media: incidence, prevention, and management. Drug Saf 1998;19:313-24.
28702 - Agrawal M, Stouffer GA. Contrast induced nephropathy after angiography. Am J Med Sci 2002;323(5):252-8.
28764 - Cipro (ciprofloxacin intravenous solution) package insert. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc.; 2022 Mar.
28879 - Pentamidine isethionate injection package insert. East Brunswick, NJ: Avet Pharmaceuticals Inc.; 2021 Jan.
29036 - Venkatakrishnan K, von Moltke LL, Greenblatt DJ. Effects of the antifungal agents on oxidative drug metabolism. Clin Pharmacokinet 2000;38:111-180.
29130 - Diovan (valsartan) tablets package insert. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2021 Apr.
29198 - Sandimmune (cyclosporine) package insert. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2023 Sept.
29202 - DDAVP (desmopressin acetate) tablets package insert. Parsippany, NJ: Ferring Pharmaceuticals Inc.; 2020 Jul.
29374 - EC Naprosyn (naproxen delayed-release) package insert. Nutley, NJ: Roche Laboratories, Inc.; 2003 May.
29558 - Ibandronate tablets package insert. Weston, FL: Apotex Corp.; 2023 Aug.
29611 - Mobic (meloxicam) tablets package insert. East Windsor, NJ: Aurobindo Pharma USA, Inc.; 2024 Dec.
29613 - Feldene (piroxicam) capsules package insert. New York, NY: Pfizer Labs; 2024 Nov.
29732 - Lovenox (enoxaparin) injection package insert. Morristown, NJ: Sanofi-Aventis U.S. LLC; 2025 May.
29747 - Riluzole tablet package insert. Bedminster, NJ: Ascend Laboratories, LLC; 2025 Mar.
29878 - Photofrin (porfimer) package insert. Birmingham, AL: Axcan Scandipharm Inc.; 2003 Aug.
29912 - Cefotaxime for injection package insert. Berkeley Heights, NJ: Hikma Pharmaceuticals USA Inc.; 2021 Jun.
29934 - Cymbalta (duloxetine hydrochloride) delayed-release capsules package insert. Indianapolis, IN: Eli Lilly and Company; 2023 Aug.
29947 - Ofloxacin Tablets package insert. Spring Valley, NY: Par Pharmaceuticals Inc.; 2003 Jun.
29960 - Nurtjahja-Tjendraputra E, Ammit AJ, Roufogalis BD, et al. Effective anti-platelet and COX-1 enzyme inhibitors from pungent constituents of ginger. Thromb Res 2003;111:259-65.
29970 - Valtrex (valacyclovir) package insert. Research Triangle Park, NC: GlaxoSmithKline; 2025 Nov.
30003 - Visudyne (verteporfin) injection package insert. Bridgewater, NJ: Bausch & Lomb Americas Inc.; 2023 Feb.
30110 - Insel PA. Analgesic-antipyretic and antiinflammatory agents and drugs employed in the treatment of gout. In: Hardman JG, Limbird LE, Molinoff PB, et al., eds. Goodman and Gilman's the pharmacological basis of therapeutics, 9th edn. New York: McGraw Hill, 1996;617-657.
30115 - Diclofenac sodium extended-release tablets package insert. Bridgewater, MJ: Bausch Health US, LLC; 2021 May.
30241 - Ansaid (flurbiprofen tablets) package insert. New York, NY: Pharmacia and Upjohn Company; 2016 May.
30242 - Tolectin® (tolmetin sodium) package insert. Spring House, PA: McNeil Pharmaceutical; 1997 Jun.
30268 - Perez Gutthann S, Garcia Rodriguez LA, Raiford DS, et al. Nonsteroidal anti-inflammatory drugs [NSAIDs] and the risk of hospitalization for acute renal failure. Arch Intern Med 1996;156(21):2433-9.
30272 - Urocit-K (potassium citrate wax matrix tablets) package insert. Mission Pharmacal Company: San Antonio, TX; 2021 Dec.
30427 - Kaufman DW, Kelly JP, Wiholm BE, et al. The risk of acute major upper gastrointestinal bleeding among users of aspirin and ibuprofen at various levels of alcohol consumption. Am J Gastroenterol 1999;94:3189-96.
30489 - Chobanian AV, Bakris GL, Black HR. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA 2003;289:2560-71.
30496 - Lodine XL (etodolac extended-release tablets) package insert. Haifa Bay, Israel: Taro Pharmaceutical Industries Ltd.; 2010 Feb.
30524 - Nalfon (fenoprofen calcium) capsule package insert. Ridgeland, MS: Xspire Pharma; 2024 Nov.
30548 - Ketoprofen capsules package insert. Ripley, MS: Misemer Pharmaceuticals, Inc.; 2024 Jul.
30555 - Tarceva (erlotinib) package insert. Northbrook, IL: OSI Pharmaceuticals, LLC; 2016 Sept.
30565 - Daypro (oxaprozin) tablet package insert. New York, NY: Pfizer, Inc.; 2024 Nov.
30569 - Ibuprofen tablets package insert. Bridgewater, NJ: Amneal Pharmaceuticals, LLC; 2023 Jun.
30570 - Mefenamic acid capsules package insert. Alpharetta, GA: Avion Pharmaceuticals; 2024 Nov.
30574 - Meclofenamate sodium capsules package insert. Morgantown, WV: Mylan Pharmaceuticals Inc.; 2024 Jul.
30676 - Emend (aprepitant oral products) package insert. Whitehouse Station, NJ: Merck & Co.,Inc.; 2019 Nov.
31027 - Pamidronate disodium injection package insert. Morgantown, WV; Mylan Institutional LLC; 2022 Jul.
31047 - Bacitracin for Injection package insert. New York, NY: Pfizer, Inc.; 2018 Apr
31230 - Baraclude (entecavir) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2019 Nov.
31807 - Exjade (deferasirox) package insert. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2020 Jul.
31826 - Ibandronate injection package insert. Weston, FL: Apotex Corp.; 2024 Sep.
31941 - Nabumetone tablet package insert. Nashville, TN: Westminster Pharmaceuticals, LLC; 2024 Aug.
31949 - Arthrotec (diclofenac sodium; misoprostol) tablets package insert. New York, NY: Pfizer, Inc.; 2024 Nov.
32018 - Ketorolac tromethamine injection package insert. Bedminster, NJ: Alembic Pharmaceuticals, Inc.; 2024 Jul.
32122 - EC Naprosyn (naproxen delayed-release tablets), Naprosyn (naproxen tablets), Anaprox DS (naproxen sodium tablets) package insert. Alpharetta, GA: Canton Laboratories, LLC; 2024 Nov.
32127 - Prozac (fluoxetine) capsules package insert. Indianapolis, IN: Eli Lilly and Company; 2023 Aug.
32159 - Visicol (sodium phosphate monobasic monohydrate; sodium phosphate dibasic anhydrous) package insert. Morrisville, NC: Salix Pharmaceuticals, Inc.; 2009 Mar.
32160 - Osmoprep (sodium phosphate monobasic monohydrate; sodium phosphate dibasic anhydrous) package insert. Bridgewater, NJ: Salix Pharmaceuticals, Inc.; 2018 Nov.
32387 - Sprycel (dasatinib) package insert. Princeton, NJ: Bristol-Myers Squibb Company; 2014 April.
32569 - Aronoff GR, Bennett WM, Berns JS, et al. Drug prescribing in renal failure: dosing guidelines for adults and children, 5th ed. Philadelphia: American College of Physicians; 2007.
32676 - Cytovene IV (ganciclovir for injection) package insert. Montgomery, AL: H2-Pharma, LLC.; 2020 Jun.
33007 - Osmitrol (mannitol) injection package insert. Deerfield, IL: Baxter Healthcare Corporation; 2019 Aug.
33200 - Tekturna (aliskiren) package insert. Orlando, FL: Noden Pharma USA Inc; 2020 Jun.
33554 - Voltaren Gel (diclofenac sodium topical gel 1%) package insert. Warren, NJ. GSK Consumer Healthcare; 2023 Feb.
33608 - Rault RM. Case report: hyponatremia associated with nonsteroidal anti-inflammatory drugs. Am J Med Sci 1993;305:318-20.
33609 - Petersson I, Nilsson G, Hansson BG, et al. Water intoxication associated with non-steroidal anti-inflammatory drug therapy. Acta Med Scand 1987;221:221-3.
33610 - Blum M, Aviram A. Ibuprofen induced hyponatraemia. Rheumatol Rehabil 1980;19:258-9.
33636 - Coly-Mycin M Parenteral (colistimethate sodium) package insert. Chestnut Ridge, NY: Par Pharmaceutical Companies, Inc.; 2015 Jul.
34408 - Zovirax (acyclovir) injection package insert. Research Triangle Park, NC: GlaxoSmithKline; 2019 Jan.
34447 - Niwa T, Shiraga T, Takagi A. Effect of antifungal drugs on cytochrome P450 (CYP) 2C9, CYP2C19, and CYP3A4 activities in human liver microsomes. Biol Pharm Bull. 2005;28:1805-1808.
34453 - Hynninen V, Olkkola KT, Leino K, et al. Effects of the antifungals voriconazole and fluconazole on the pharmacokinetics of S-(+)- and R-(-)-ibuprofen. Antimicrob Agents Chemother 2006;50:1967-72.
34454 - Hamman MA, Thompson GA, Hall SD. Regioselective and stereoselective metabolism of ibuprofen by human cytochrome P450 2C. Biochem Pharmacol 1997;54;1:33-41.
34461 - Pilotto A, Seripa D, Franceschi M, et al. Genetic susceptibility to nonsteroidal anti-inflammatory drug-related gastroduodenal bleeding: role of cytochrome P450 2C9 polymorphisms. Gastroenterol 2007;133:465-71.
34462 - Kirchheiner J, Meineke I, Freytag G, et al. Enantiospecific effects of cytochrome P450 2C9 amino acid variants on ibuprofen pharmacokinetics and on the inhibition of cyclooxygenases 1 and 2. Clin Pharmacol Ther 2002;72:62-75.
35581 - Deplin (L-methylfolate) capsules package insert. Shreveport, LA: Alfasigma USA, Inc.; 2024 Feb.
35603 - Li G, Treiber G, Maier K, et al. Disposition of ibuprofen in patients with liver cirrhosis Stereochemical considerations. Clin Pharmacokinet 1993;25:154-63.
35893 - Caldolor (ibuprofen) injection package insert. Nashville, TN: Cumberland Pharmaceuticals; 2024 Nov.
36055 - Effient (prasugrel) package insert. South Plainfield, NJ: Cosette Pharmaceuticals, Inc.; 2022 Feb.
36615 - Vibativ (telavancin) package insert. Nashville, TN: Cumberland Pharmaceuticals Inc.; 2020 July.
36890 - Folotyn (pralatrexate) package insert. Westminster, CO: Allos Therapeutics; 2011 Jan.
38831 - Oleptro (trazodone hydrochloride) extended-release tablets package insert. Dublin, Ireland: Labopharm Europe Limited; 2014 Jul.
39165 - Prevnar 13 (pneumococcal 13-valent conjugate vaccine) package insert. Philadelphia, PA: Wyeth Pharmaceuticals Inc.; 2017 Aug.
40027 - Emend (fosaprepitant dimeglumine injection) package insert. Whitehouse Station, NJ: Merck & Co.,Inc.; 2022 May.
40392 - Promacta (eltrombopag) package insert. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2025 Jun.
40621 - Tinzaparin (Innohep) solution for injection. Parsippany, New Jersey: Leo Pharma Incorporated; 2010 May.
41139 - Novantrone (mitoxantrone) package insert. Rockland, MA; Sereno Inc: 2010 Jun.
41237 - Tegretol (carbamazepine) package insert. East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2025 Sept.
41251 - Bone KM: Potential interaction of Ginkgo biloba leaf with antiplatelet or anticoagulant drugs: what is the evidence. Mol Nutr Food Res 2008;52(7):764-771.
41258 - Aruna LL, Naidu MU. Pharmacodynamic interaction studies of Ginkgo biloba with cilostazol and clopidogrel in healthy human subjects. Br J Clin Pharmacol 2006;63:333-338.
41265 - Engelsen J, Nielsen JD, Winter K. Effect of coenzyme Q10 and Ginkgo biloba on warfarin dosage in patients on long-term warfarin treated outpatients; a randomised, double blind, placebo-crossover trial. Thromb Haemost 2002;87:1075-6.
41573 - Suprep (sodium sulfate, potassium sulfate, and magnesium sulfate) oral solution concentrate package insert. Braintree, MA: Braintree Laboratories, Inc.; 2025 Nov.
41826 - Zevalin (ibritumomab tiuxetan) package insert. Irvine, CA: Spectrum Pharmaceuticals, Inc.; 2019 Sept.
41853 - Proleukin (aldesleukin) package insert. Malvern, PA: Clinigen, Inc.; 2023 Sept.
42080 - Atelvia (risedronate sodium) delayed-release tablet package insert. North Chicago, IL: AbbVie Inc.; 2023 Oct.
42121 - Pradaxa (dabigatran) oral capsules package insert. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc.; 2025 Jun.
42968 - Photofrin (porfimer sodium) package insert. Bannockburn, IL: Pinnacle Biologics, Inc.; 2020 Jan.
43177 - Viibryd (vilazodone) tablets package insert. Madison, NJ; Allergan USA, Inc.: 2024 Apr.
43411 - Cipro (ciprofloxacin tablet; suspension) package insert. Whippany, NJ: Bayer HealthCare Pharmaceuticals Inc.; 2024 Sept.
44120 - IBU (ibuprofen) tablets package insert. Princeton, NJ: Dr. Reddy's Laboratories, Inc.; 2024 Jul.
44121 - Ibuprofen oral suspension package insert. East Windsor, NJ: Aurobindo Pharma USA, Inc.; 2024 Aug.
44130 - Duexis (ibuprofen and famotidine) tablets package insert. Deerfield, IL: Horizon Medicines, LLC.; 2024 Nov.
44155 - Capastat (capreomycin sulfate injection) package insert. Lake Forest, IL: Akorn, Inc.; 2023 Jan.
45335 - Zelboraf (vemurafenib) tablet package insert. South San Francisco, CA: Genentech USA, Inc.; 2020 May.
45875 - Etodolac package insert. Camarillo, CA: GSMS Inc.; 2008 Dec.
45886 - Indocin (indomethacin) oral suspension package insert. Wayne, PA: Zyla Life Sciences US, Inc.; 2024 Nov.
48492 - Huerta C, Castellsague J, Varas-Lorenzo C, Garcia Rodriguez LA. Nonsteroidal anti-inflammatory drugs and risk of ARF in the general population. Am J Kidney Dis 2005;45(3):531-539.
48524 - Kalydeco (ivacaftor) package insert. Boston, MA: Vertex Pharmaceuticals Incorporated; 2025 Sep.
48697 - Korlym (mifepristone) tablet package insert. Menlo Park, CA: Corcept Therapeutics; 2019 Nov.
49143 - Dolobid (diflunisal) tablet package insert. Fairmont, WV: INA Pharmaceuticals, Inc.; 2024 Nov.
49634 - Arava (leflunomide) package insert. Bridgewater, NJ:. Sanofi-Aventis U.S. LLC; 2024 Jun.
49946 - Fragmin (dalteparin) injection. New York, NY: Pfizer, Inc.; 2024 Oct.
49952 - Fibricor (fenofibric acid) package insert. Athens, GA: Athena Bioscience LLC.; 2025 Jun.
51000 - Clinoril (sulindac) package insert. Whitehouse Station, NJ: Merck Co., Inc.; 2007 Feb.
51258 - Prepopik (Sodium picosulfate; magnesium oxide; anhydrous citric acid) package insert. Parsippany, NJ: Ferring Pharmaceuticals Inc.; 2018 Aug.
51664 - Stribild (elvitegravir; cobicistat; emtricitabine; tenofovir disoproxil fumarate) package insert. Foster City, CA: Gilead Sciences, Inc; 2021 Sept.
52213 - Synribo (omacetaxine mepesuccinate) injection package insert. North Wales, PA:Teva Pharmaceuticals USA, Inc.; 2019 Nov.
52249 - Binosto (alendronate sodium) effervescent tablets for oral solution package insert. Boston, MA: Radius Health, Inc.; 2023 Oct.
52739 - Eliquis (apixaban) package insert. Bristol-Myers Squibb Company; Princeton, NJ. 2025 Apr.
53719 - Curhan SG, Eavey R, Shargorodsky J, et al. Analgesic use and the risk of hearing loss in men. Am J Med 2010;123:231-237.
53720 - Curhan SG, Shargorodsky J, Eavey R, et al. Analgesic use and the risk of hearing loss in women. Am J Epidemiol 2012;176:544-554.
53793 - Potassium chloride oral solution package insert. Allentown, PA: Genus Lifesciences Inc.; 2019 July.
54023 - Litalien C, Jacqz-Aigrain E. Risks and benefits of nonsteroidal anti-inflammatory drugs in children: a comparison with paracetamol. Paediatr Drugs 2001;3:817-858.
54241 - Lithium carbonate tablets, capsules, and oral solution package insert. Eatontown, NJ: West-Ward Pharmaceuticals Corp.; 2018 Dec.
55079 - Rainsford KD. Ibuprofen: pharmacology, efficacy, and safety. Inflammopharmacology 2009;17:275-342.
55084 - Lands LC, Milner R, Cantin AM, et al. High-dose ibuprofen in cystic fibrosis: Canadian safety and effectiveness trial. J Pediatr 2007;151:249-254.
55086 - Dlugosz CK, Chater RW, Engle JP. Appropriate use of nonprescription analgesics in pediatric patients. J Pediatr Health Care 2006;20:316-325.
55095 - Motrin IB (ibuprofen) tablets package insert (OTC). Fort Washington, PA: Johnson & Johnson Consumer Inc., McNeil Consumer Healthcare Division; 2017 Apr.
55102 - Giannini EH, Brewer EJ, Miller ML, et al. Ibuprofen suspension in the treatment of juvenile rheumatoid arthritis. Pediatric Rheumatology Collaborative Study Group. J Pediatr 1990;117:645-652.
55106 - Rose CD, Doughty RA. Pharmacological management of juvenile rheumatoid arthritis. Drugs 1992;43:849-863.
55107 - Steans A, Manners PJ, Robinson IG. A multicentre, long-term evaluation of the safety and efficacy of ibuprofen syrup in children with juvenile chronic arthritis. Brit J Clin Pract 1990;44:172-175.
55469 - Fetzima (levomilnacipran) extended-release capsules package insert. North Chicago, IL: AbbVie, Inc.; 2024 Apr.
55688 - O'Gara P, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e362-e425.
56041 - Trintellix (vortioxetine tablets) package insert. Lexington, MA: Takeda Pharmaceuticals America, Inc.; 2023 Aug.
56074 - Duavee (conjugated estrogens and bazedoxifene) package insert. Philadelphia, PA: Wyeth Pharmaceuticals Inc.; 2024 March.
56263 - Otrexup (methotrexate) injection for subcutaneous use package insert. Ewing, NJ: Antares Pharma, Inc.:2019 Dec.
56268 - Celebrex (celecoxib) package insert. Morgantown, WV; Viatris Specialty LLC; 2024 Nov.
56767 - Mogayzel PJ, Naureckas ET, Robinson KA. Cystic fibrosis pulmonary guidelines: chronic medications for maintenance of lung health. Am J Respir Crit Care Med 2013;187:680-689.
57694 - Quin JD. The nephrotoxicity of cephalosporins. Adverse Drug React Acute Poisoning Rev 1989;8:63-72.
57695 - Rankin GO, Sutherland CH. Nephrotoxicity of aminoglycosides and cephalosporins in combination. Adverse Drug React Acute Poisoning Rev 1989;9:73-88.
57741 - Orbactiv (oritavancin) package insert. Lincolnshire, IL: Melinta Therapeutics, LLC; 2022 Jan.
57771 - Rasuvo (methotrexate) injection for subcutaneous use, package insert. Chicago, IL: Medexus Pharma Inc. 2020 Mar.
58001 - Vitekta (elvitegravir) package insert. Foster City, CA: Gilead Sciences, Inc; 2015 Jul.
58208 - Zhanel GG. Cephalosporin-induced nephrotoxicity: does it exist? DICP 1990;24:262-5.
58724 - Zoledronic acid injection package insert. Columbus, OH: BluePoint Laboratories; 2020 Jun.
59891 - Orkambi (lumacaftor; ivacaftor) tablet package insert. Boston, MA: Vertex Pharmaceuticals, Inc. 2025 Sep
59937 - US Food and Drug Administration (FDA). Non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDS): Drug Safety Communication - association with heart attacks or strokes. Retrieved July 9, 2015. Available on the World Wide Web at: http://www.fda.gov/downloads/Drugs/DrugSafety/UCM453941.pdf
60122 - Keveyis (dichlorphenamide) tablets package insert. Trevose, PA: Strongbridge US Inc.; 2019 Nov.
60362 - Rigourd V, de Villepin B, Amirouche A, et al. Ibuprofen concentrations in human mature milk-first data about pharmacokinetics study in breast milk with AOR-10127 "Antalait" study. Ther Drug Monit 2014;36:590-596.
60438 - Durlaza (aspirin extended-release capsule) prescribing information. North Haven, CT; New Haven Pharmaceuticals: 2015 Sept.
60439 - Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA. 2015;314:1498-1506. Review. Erratum in: JAMA. 2015;314:1978.
60517 - Methotrexate injection solution package insert. Lake Forrest, IL: Hospira Inc; 2025 May.
60860 - Byvalson (nebivolol and valsartan) tablets package insert. Irvine, CA: Allergan USA, Inc.; 2023 Jun.
61088 - Zorvolex (diclofenac) capsules package insert. Wayne, PA: Zyla Life Sciences US, Inc.; 2024 Nov.
61171 - Yosprala (aspirin and omeprazole delayed-release tablets) package insert. Allentown, PA: Genus Lifesciences, Inc.; 2024 Nov.
61325 - Prinivil (lisinopril) tablets package insert. Whitehouse Station, NJ: Merck & Co., Inc. 2021 Nov.
61413 - Vemlidy (tenofovir alafenamide) package insert. Foster City, CA: Gilead Sciences, Inc.; 2024 March.
61900 - Xatmep (methotrexate) oral solution package insert.Wilmington, MA: Azurity Pharmaceuticals, Inc.; 2020 Mar.
62206 - Kidney Disease Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl 2013;3:1-150
62723 - Macrilen (macimorelin) package insert. Frankfurt am Main, Germany: Aeterna Zentaris GmbH; 2018 Jan.
63000 - Sullivan JE, Farrar HC, et al. Fever and antipyretic use in children. Pediatrics 2011;127:580-587.
63043 - Tattelman E. Health effects of garlic. Am Fam Physician. 2005;72:103-106. Review.
63549 - Bjornsson ES. Hepatotoxicity by drugs: the most common implicated agents. Int J Mol Sci 2016;17:224.
63624 - Tegsedi (inotersen) injection package insert. Waltham, MA: Akcea Therapeutics, Inc.; 2024 Jan.
63923 - 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71:2052-2081
64014 - Qmiiz (meloxicam) orally disintegrating tablet. Deerfield, IL: TerSera Therapeutics, LLC; 2021 Apr.
64373 - Qaseem A, Harris RP, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Management of Acute and Recurrent Gout: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166:58-68.
64535 - Turalio (pexidartinib) capsules package insert. Basking Ridge, NJ: Daiichi Sankyo, Inc.; 2025 Jan.
64561 - Pretomanid tablet package insert. Hyderabad, India: Mylan, Laboratories Limited; 2024 Nov.
64565 - Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: The American Headache Society evidence assessment of migraine pharmacotherapies. Headache 2015;55:3-20.
64587 - Oskoui M, Pringsheim T, Holler-Managan Y, et al. Practice guideline update summary: Acute treatment of migraine in children and adolescents: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 2019;93:487-499.
65562 - Levofloxacin tablets package insert. Piscataway, NJ: Camber Pharmaceuticals, Inc.; 2024 July.
66040 - Food and Drug Administration MedWatch. Nonsteroidal anti-inflammatory drugs (NSAIDs): Drug safety communication - avoid use of NSAIDs in pregnancy at 20 weeks or later. Available at: https://www.fda.gov/safety/medical-product-safety-information/nonsteroidal-anti-inflammatory-drugs-nsaids-drug-safety-communication-avoid-use-nsaids-pregnancy-20. Accessed October 15, 2020.
66336 - Lupkynis (voclosporin) capsules package insert. Rockville, MD: Aurinia Pharma U.S., Inc.; 2025 Oct.
66357 - Baker M, Perazella MA. NSAIDs in CKD: Are they safe? Am J Kidney Dis 2020;76:546-557.
66574 - Advil Migraine (ibuprofen) capsule package insert. Warren, NJ: GlaxoSmithKline Consumer Healthcare; 2021 Sep.
66594 - Methotrexate tablets package insert. Parsippany, NJ: Teva Pharmaceuticals USA, Inc.; 2023 Aug
66767 - Diener HC, Antonaci F, Braschinsky M, et al. European Academy of Neurology guideline on the management of medication overuse headache. Eur J Neurol 2020;27:1102-1116.
66803 - Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.
66830 - Ibuprofen chewable tablet (Junior Strength Advil) package insert. Warren, NJ: GlaxoSmithKline Consumer Healthcare Holdings (US) LLC; 2020 Nov.
66831 - Children's Advil (ibuprofen suspension) package insert. Warren, NJ: GlaxoSmithKline Consumer Healthcare Holdings (US) LLC; 2021 Jul.
66832 - Ibuprofen concentrated suspension/drops (Infants Advil) package insert. Warren, NJ: GlaxoSmithKline Consumer Healthcare Holdings (US) LLC; 2020 Nov.
67147 - Pemfexy (pemetrexed) injection package insert. Woodcliff Lake, NJ: Eagle Pharmaceuticals, Inc; 2022 Dec.
67418 - Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines on the diagnosis and management of pericardial diseases. Eur Heart J. 2015;36:2921-2964.
67419 - Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines on the diagnosis and management of pericardial diseases - Web Addenda. Eur Heart J. 2015; doi:10.1093/eurheart/ehv318
68127 - Castellani C, Duff AJA, Bell SC, et al. ECFS best practice guidelines: the 2018 revision. J Cyst Fibros 2018;17:153-78.
68641 - Sparsentan (Filspari) package insert. San Diego, CA: Travere Therapeutics, Inc.; 2025 Aug.
69288 - Ailani J, Burch RC, Robbins MS; Board of Directors of the American Headache Society. The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice. Headache 2021;61:1021-1039.
70364 - Drugs and Lactation Database (LactMed) [e-book]. Bethesda (MD): National Institute of Child Health and Human Development; 2006- . Available from: https://www.ncbi.nlm.nih.gov/books/NBK501922/. Accessed February 21, 2024.
70365 - Hales TW, Krutsch K. Hale’s Medications and Mother’s Milk. 20th ed.[e-book]. New York City: Springer Publishing; 2023. Available from: https://www.halesmeds.com/. Accessed February 21, 2024.
70571 - Beqvez (fidanacogene elaparvovec) injection package insert. New York, NY: Pfizer Inc.; 2024 Apr.
71081 - McIntosh SE, Freer L, Grissom CK, et al. Wilderness Medical Society Clinical Practice Guidelines for the Prevention and Treatment of Frostbite: 2024 Update. Wilderness Environ Med 2024;35:183-197
71453 - Chiabrando JG, Bonaventura A, Vecchie A, et al. Management of Acute and Recurrent Pericarditis: JACC State-of-the-Art review. J Am Coll Cardiol 2020;75(1):76-92.
71619 - American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins-Gynecology. ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent. Obstet Gynecol 2018;132(6):e249-e258.
71620 - Ferris-Rowe E, Corey E, Archer JS. Primary dysmenorrhea: diagnosis and therapy. Obstet Gynecol 2020;136(5):1047-1058.
71829 - Klomjit N, Ungprasert P. Acute kidney injury associated with non-steroidal anti-inflammatory drugs. Eur. J. Intern. Med. 2022;101:21-8.
72005 - RHDAustralia (ARF/RHD writing group). The 2020 Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease (3.2 edition, March 2022). Accessed March 5, 2025. Available at https://www.rhdaustralia.org.au/system/files/fileuploads/arf_rhd_guidelines_3.2_edition_march_2022.pdf
72025 - Mocumbi AO. Rheumatic Fever. In: Libby P, Bonow RO, Mann DL, et al, eds. Braunwald's Heart Disease: a Textbook of Cardiovascular Medicine, 12th edition. Philadelphia, PA: Saunders, an imprint of Elsevier; 2022:1513-1539.
72477 - Wan EYF, et al. Comparative Risks of Nonsteroidal Anti-Inflammatory Drugs on CKD. Clin J Am Soc Nephrol. 2021 Jun;16(6):898-907.
72681 - Luks AM, Beidleman ScD, Freer L, et al. Wilderness Medical Society clinical practice guidelines for the prevention, diagnosis, and treatment of acute altitude illness: 2024 update. Wilderness Environ Med 2024;35(1S):2S-19S.
72682 - Hackett PH, Shlim DR. High-altitude travel and altitude illness. In: CDC Yellow Book: Health Information for International Travel, 2026. Accessed September 19. 2025. Available on the World Wide Web at https://www.cdc.gov/yellow-book/hcp/environmental-hazards-risks/high-altitude-travel-and-altitude-illness.html.