Quick Facts
Location: Abdominal cavity.
Arterial Supply: Branches of the celiac trunk (gastroduodenal and superior pancreaticoduodenal arteries) and superior mesenteric artery (inferior pancreaticoduodenal, jejunal, ileal, ileocecal arteries).
Venous Drainage: Superior and inferior pancreaticoduodenal vein, draining to the portal vein and superior mesenteric vein, respectively.
Innervation: Parasympathetic: Vagus nerve (CN X); Sympathetic: celiac ganglia; Visceral afferents: spinal ganglia of T5-T9; Enteric innervation.
Lymphatic Drainage: Pyloric and pancreaticoduodenal lymph nodes, to celiac and superior mesenteric lymph nodes.
Related parts of the anatomy
Structure/Morphology
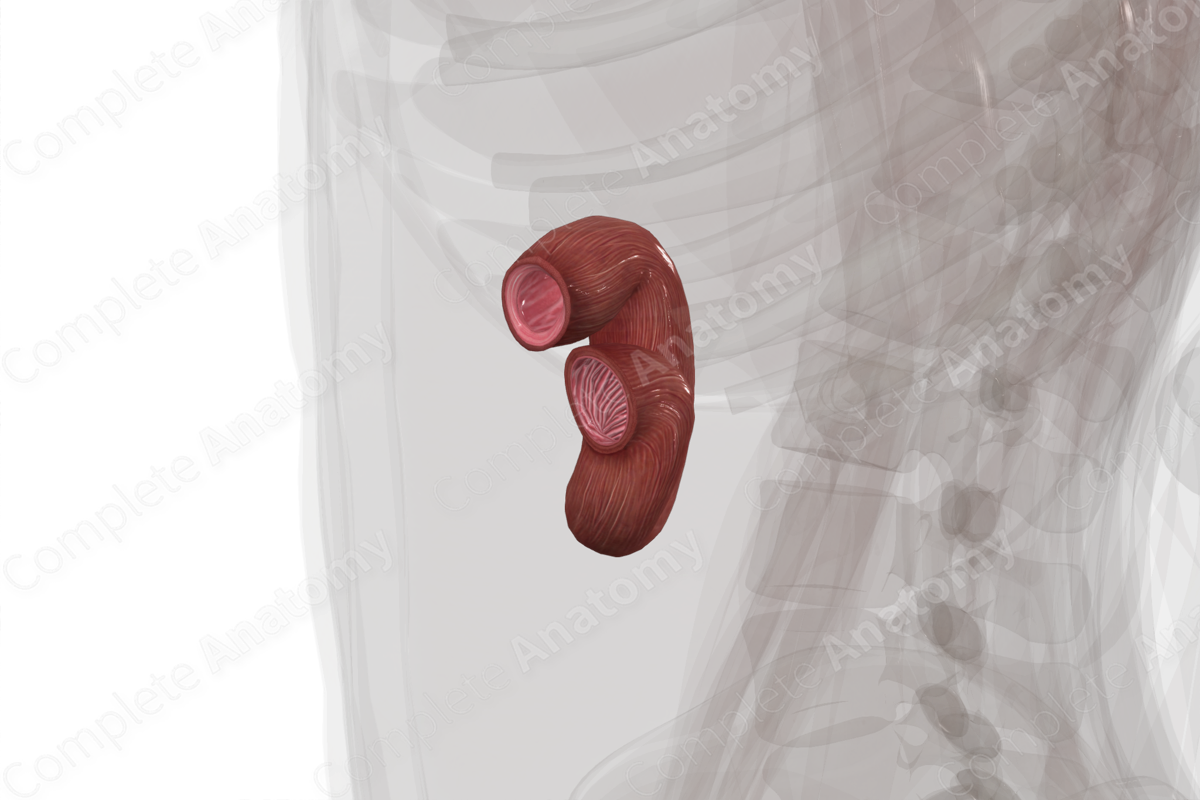
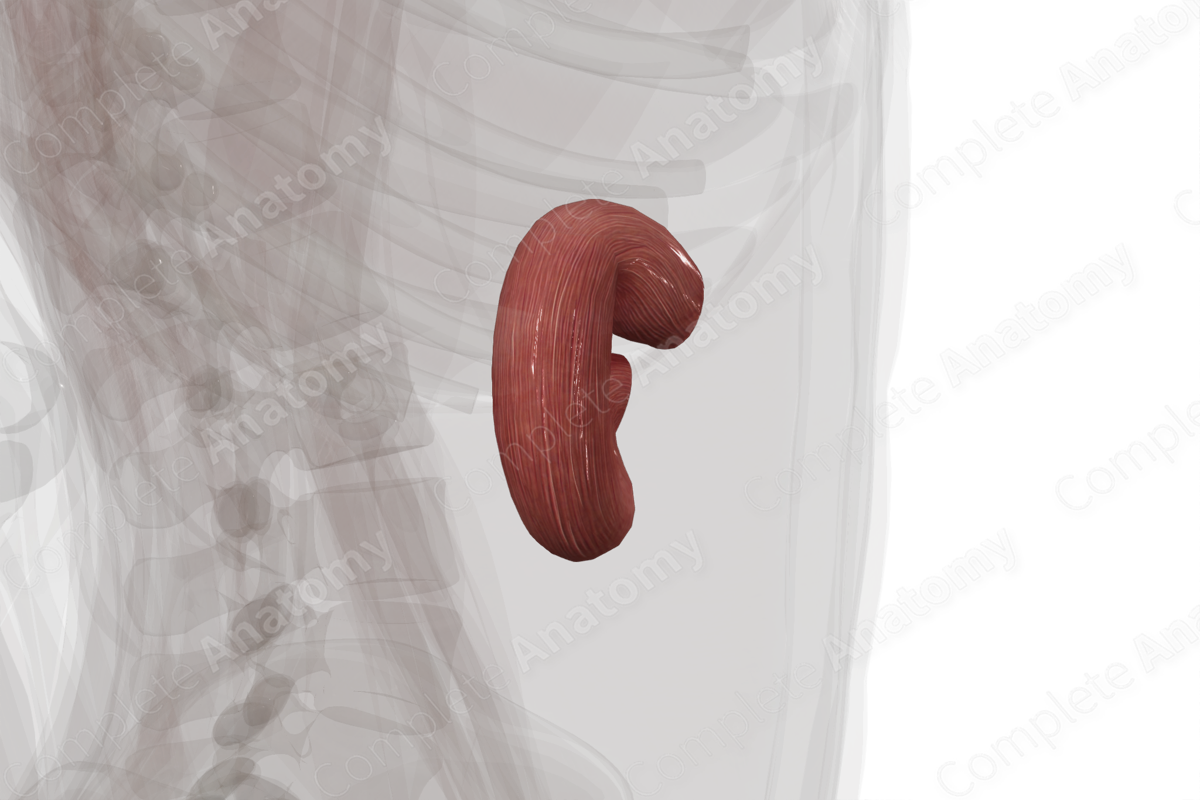
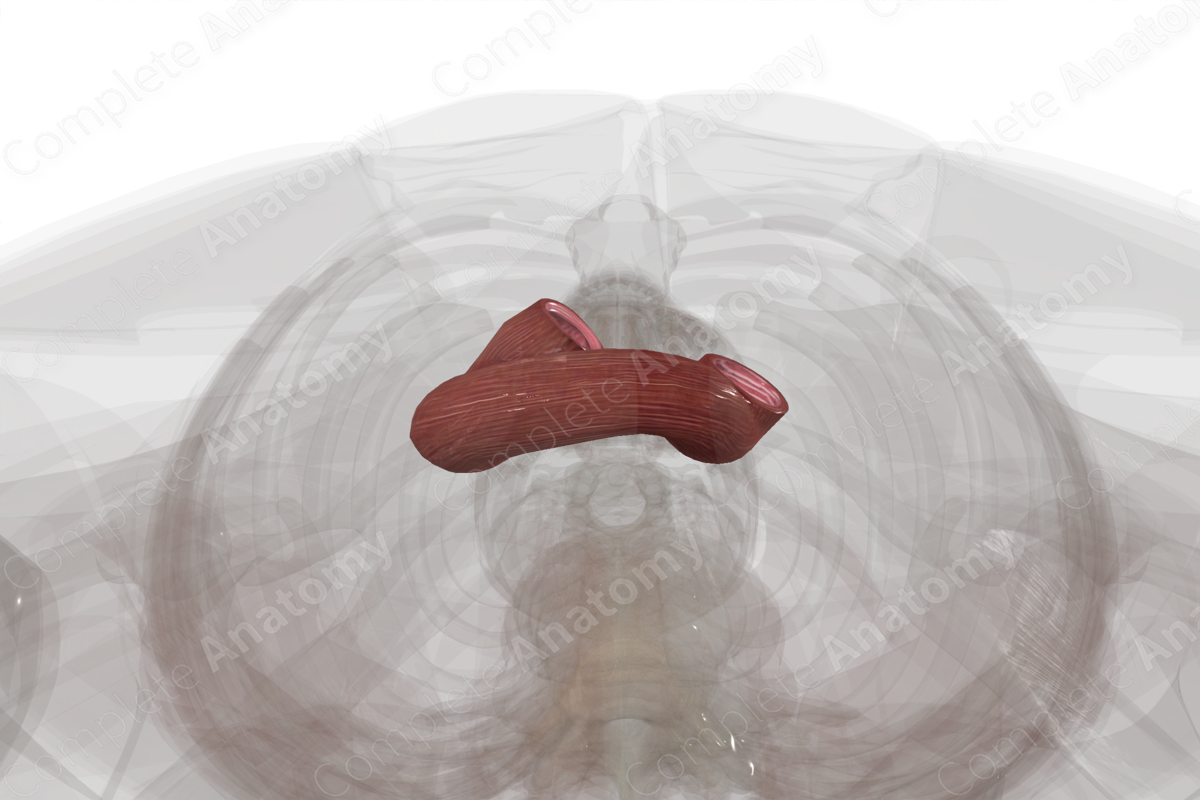
The duodenum is made up of four primary segments: superior, descending, horizontal, and ascending duodenum. These are also known as the first, second, third, and fourth parts of the duodenum, respectively.
The cross-sectional microarchitecture of the duodenum demonstrates mucosa, submucosa, and muscular (inner circular and outer longitudinal) layers with a thin outer serosal covering (Standring, 2016).
The superior and descending colon are related to the foregut while the horizontal and ascending segments of the duodenum are related to the midgut. This developmental distinction is important in understanding the patterns of vascularization, innervation, and lymphatic drainage of the duodenum.
Anatomical Relations
The duodenum is the shortest part of the small intestine, forming a roughly C-shaped structure around the head of the pancreas.
The superior portion of the duodenum begins on the distal side of the pyloric sphincter roughly ventral to the L1 vertebra. The initial part, called the duodenal cap, is intraperitoneal and covered by a mesentery. Shortly thereafter, the superior duodenum dives posteriorly to become retroperitoneal. The superior duodenum is anterior to the bile duct and neck of the pancreas, and posterior to the gallbladder and quadrate lobe of the liver. It’s the portion to which the heaptoduodenal ligament attaches to form the omental (epiploic) foramen.
The descending portion of the duodenum runs inferiorly along the right edge of the pancreas, from L1 to L3 vertebral levels. It remains retroperitoneal. It passes posterior to the transverse colon and transverse mesocolon, and anterior to the hilum of the right kidney and the right ureter. Bile and pancreatic secretions enter the descending portion of the duodenum via the major duodenal papilla. A variably present minor duodenal papilla also transmits pancreatic enzymes from the accessory pancreatic duct.
The horizontal portion of the duodenum runs medially at the L3 vertebral level. It crosses posterior to the superior mesenteric artery and vein and anterior to the aorta. It courses inferior to the head of the pancreas and across to the left side of the L3 vertebra.
The ascending duodenum runs superiorly to the left of the aorta a few centimeters until turning ventrally when it reaches the body of the pancreas at the L2 vertebral level. Here it becomes intraperitoneal and ends at the duodenojejunal junction. The distal end of the duodenum is attached to the suspensory muscle of the duodenum (or ligament of Treitz), a muscular band extending from the right crus of the diaphragm (Moore, Dalley and Agur, 2013).
Function
The duodenum is primarily a site of digestion.
Chyme that enters the duodenum from the stomach is neutralized with alkaline mucus secreted by Brunner’s glands of the duodenal mucosa or bicarbonate secreted by the pancreas.
Entry of chyme into the duodenum also triggers hormonal feedback to:
- the stomach to slow gastric emptying;
- the liver and gallbladder to secrete bile which aids in the emulsification and absorption of lipids;
- the pancreas which releases pancreatic juices for enzymatic digestion of proteins, carbohydrates, fats, and nucleic acids (Sircar, 2016).
The duodenum is also a site of absorption. It absorbs nonheme iron, sugars, peptides, fats, calcium, and phosphate. Water can move either in or out of the duodenum depending on whether chyme is hypo- or hypertonic.
Arterial Supply
The duodenum is supplied by both the celiac trunk and the superior mesenteric artery.
From the celiac trunk, the gastroduodenal artery is a branch of the hepatic artery and serves the proximal portion of the duodenum. It directly gives rise to branches that serve the duodenal cap. The superior pancreaticoduodenal artery is a terminal branch of the gastroduodenal artery. This in turn splits to form both anterior and posterior pancreaticoduodenal arteries that supply blood to the anterior and posterior surfaces of the duodenum. The superior and descending portions of the duodenum, typically down to the area around the major duodenal papilla are supplied by these branches.
The duodenal tissue supplied by the superior pancreaticoduodenal arteries marks the extent of the foregut. This vasculature anastomoses with vessels from the inferior pancreaticoduodenal arteries which are associated with the midgut.
The superior mesenteric artery gives rise to the inferior pancreaticoduodenal artery. This bifurcates to form both anterior and posterior branches, which supply the anterior and posterior portions of the distal duodenum. Typically this covers duodenal tissue from the major duodenal papilla to the duodenojejunal juncture.
Venous Drainage
The venous drainage is into the portal circulation. The pattern largely parallels the arterial supply.
Blood draining via the posterior superior pancreaticoduodenal vein typically drains into the portal vein. The anterior superior pancreaticoduodenal vein and both the anterior and posterior inferior pancreaticoduodenal veins in contrast drain into the superior mesenteric vein.
Innervation
Innervation of the duodenum includes the enteric nervous system (sensory and motor), the autonomic nervous system (sympathetic and parasympathetic), and the extrinsic sensory innervation (visceral afferents) (Standring, 2016).
The vagus nerve (CN X) provides parasympathetic innervation to the duodenum.
Sympathetic innervation originates in the T5-T9 spinal cord levels with preganglionic neurons. The duodenum is supplied by postganglionic neurons from the celiac plexus.
Visceral afferent nerves from the duodenum ascend along the vagus nerve or greater splanchnic nerve (Qin et al., 2007).
The enteric system consists of two plexuses of densely packed small neurons. Meissner’s plexus lies in the submucosal layer and Auerbach’s myenteric plexus lie between the outer longitudinal and inner circular smooth muscle layers. These systems of nerves control mucosal and peristaltic function.
Lymphatic Drainage
Lymphatic drainage from the duodenum parallels the arterial supply and drains into celiac and superior mesenteric lymph nodes (Földi et al., 2012).
The pyloric nodes drain the proximal duodenum to the celiac trunk. The anterior and posterior pancreaticoduodenal lymph nodes drain to either the celiac or superior mesenteric lymph nodes. Ultimately all lymph drains via the celiac trunk to the cisterna chyli.
List of Clinical Correlates
- Gastroenteritis
- Crohn’s disease
- Peptic ulcers
- Duodenitis
- Celiac disease
References
Földi, M., Földi, E., Strößenreuther, R. and Kubik, S. (2012) Földi's Textbook of Lymphology: for Physicians and Lymphedema Therapists. Elsevier Health Sciences.
Moore, K. L., Dalley, A. F. and Agur, A. M. R. (2013) Clinically Oriented Anatomy. Clinically Oriented Anatomy 7th edn.: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Qin, C., Chen, J. D., Zhang, J. and Foreman, R. D. (2007) 'Duodenal afferent input converges onto T9-T10 spinal neurons responding to gastric distension in rats', Brain Res, 1186, pp. 180-7.
Sircar, S. (2016) Principles of Medical Physiology. 2nd edn.: Thieme.
Standring, S. (2016) Gray's Anatomy: The Anatomical Basis of Clinical Practice. Gray's Anatomy Series 41 edn.: Elsevier Limited.
Learn more about this topic from other Elsevier products