For the benefit of every patient
Our goal is the same as yours: improve outcomes for every patient. Let’s do it together.

A bright future for health
Elsevier Health sees a bright future for global health. And it’s a future that we’re building together. Where we unite in our reliance on science and trusted medical information; where students become practice-ready professionals; where every patient is treated equally and fairly; where data-driven advancements improve outcomes and where clinicians can identify the most optimal treatment for every patient.
Why do we do this? The same reason you do. For the benefit of every patient.
Products for Clinicians and Educators
For Physicians
Support evidence-based decisions with credible, comprehensive content.
Featured products:

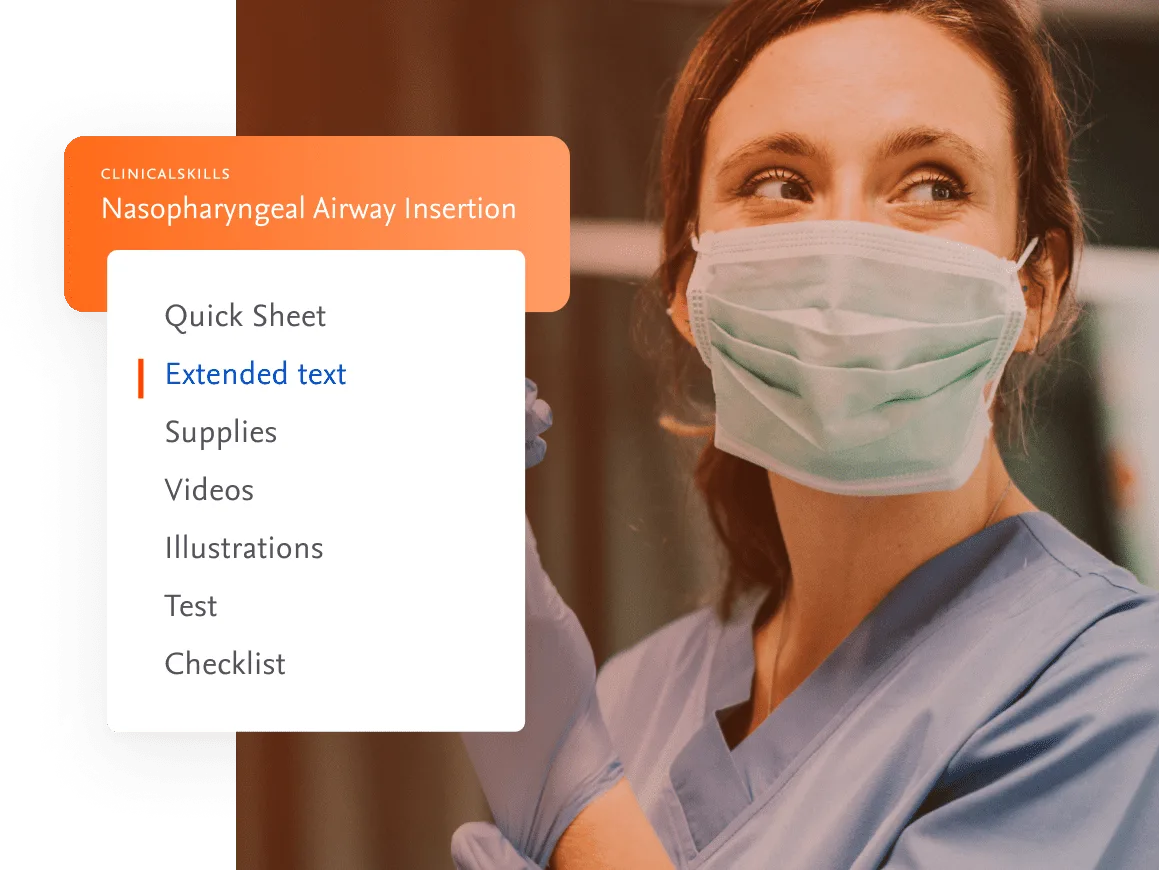
For Nurses
Empower nurses and patients with trusted, evidence-based information.
Featured products
For Medical Faculty
Support educators with learning that integrates with your teaching and engages your students.
Featured products:
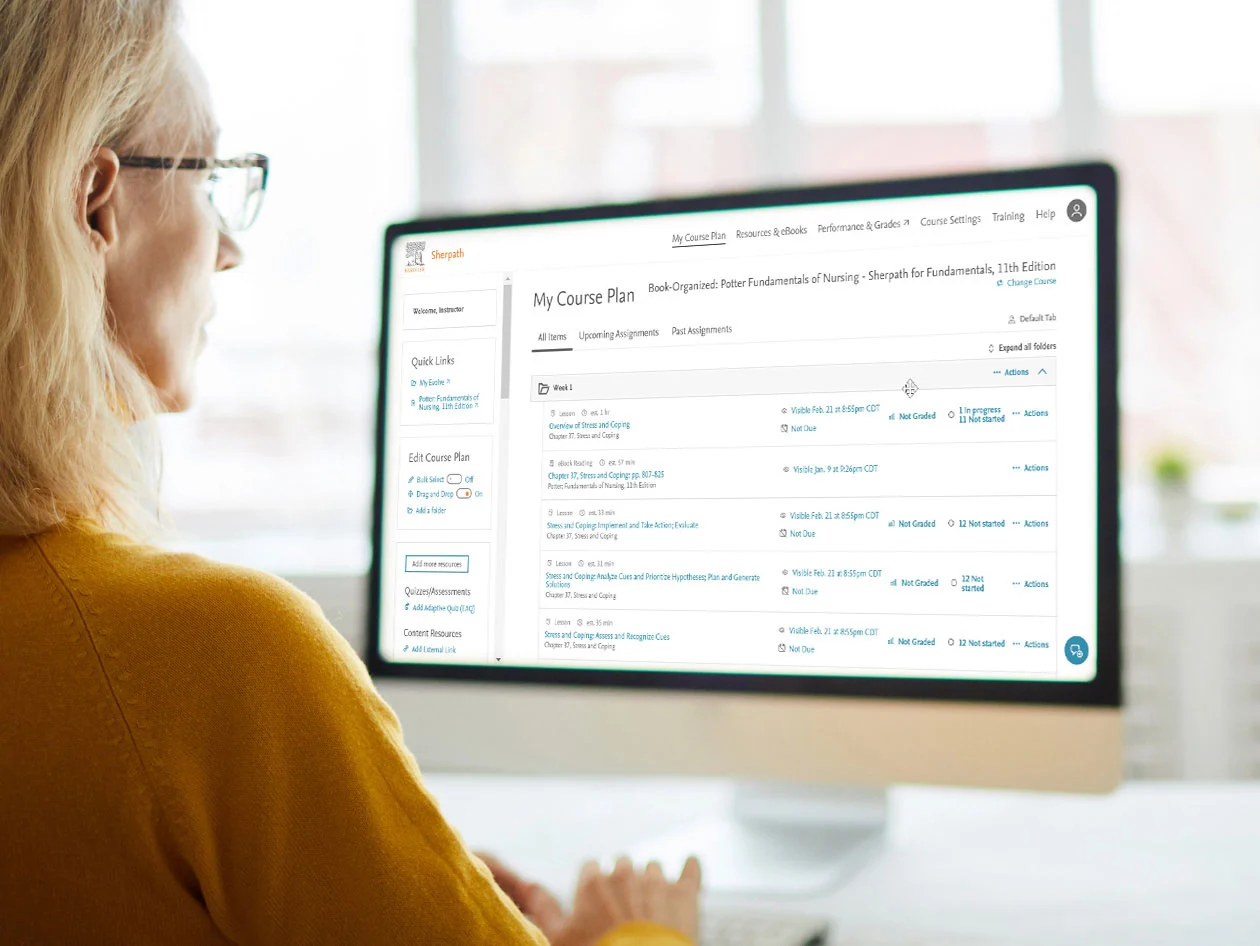
For Nurse Faculty
Our nursing resources are designed to help meet your program goals and ensure students are practice-ready.
Recommended products:
Supporting you in healthcare
Nurses
Empowering nurses with trusted resources for clinical answers
Physician
Providing physicians with the evidence-based information you need
Pharmacist
Supporting pharmacists with making informed decisions on medication alternatives and patient engagement.
Medical Faculty
Teach, train and stay current on the latest evidence-based information.
Medical Students
Discover how Elsevier supports today’s students to be tomorrow’s physicians
Nursing Students
Preparing students to provide safe and effective nursing care.
Nursing Faculty
Our nursing resources are designed to help meet your program goals and ensure students are practice-ready.